https://meditropics.com/polyneuritis-cranialis-atypical-gbs/
* Renu Kumawat
*Senior Resident, Department of Medicine, Lady Hardinge Medical College, New Delhi
A 29-years old stenographer from Bihar, India presented with complaints of difficulty in lifting left arm, difficulty in swallowing food and hoarseness of voice for 10 days. Patient is non vegetarian by diet. He had history of left sided Bell’s palsy one year back, for which he took treatment, with no residual paralysis. He had no other comorbidities. There was a history of Covid-19 vaccination one year back. He had no history suggestive of substance use. His family history was suggestive of ADPKD in his father, uncle and elder brother.
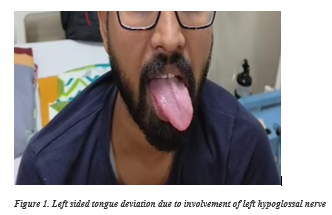
On examination, patient had a GCS = E4V5M6, pulse rate of 84/min, BP= 150/80 mmHg, RBS= 121 mg/dl and was maintaining a saturation of 98% on room air with the respiratory rate of 16/min. There was no pallor, icterus, cyanosis, clubbing, lymphadenopathy or pedal edema. Central nervous system examination was suggestive of left sided lower motor neuron palsy of cranial nerve ninth, tenth, eleventh and twelfth. Rest of the CNS examination including motor, sensory and cerebellar functions were normal. He was diagnosed with hypertension during the hospital stay. Rest of the systemic examination was within normal limits.
He was worked up for the above-mentioned complaints. Patient’s blood investigations i.e. CBC, LFT, KFT, VBG and lipid profile were within normal limits. His HIV, HBsAg and Anti-HCV were non-reactive. Chest X-ray and ECG were grossly normal. The patient’s iPTH levels, HbA1c, thyroid profile, vitamin B12, folic acid, vitamin D levels and coagulation profile were within normal limits. ANA by immunofluorescence, c ANCA and p ANCA were performed for autoimmune disorders and vasculitis which were negative. Urine investigations- routine microscopy, albumin-creatinine ratio, protein-creatinine ratio and electrolytes were normal. Serum protein electrophoresis was performed that showed hypergammaglobulinemia.
CECT head and neck was performed which revealed medialisation of the posterior half of the left vocal cord forming soft tissue projection in the airway depicting left vocal cord palsy. On the left side, the base of the tongue appeared to be protruding into the left vallecula likely to be due to left hypoglossal nerve palsy.
CE MRI brain along with the screening of whole spine did not reveal any abnormality. NCV of upper limb and lower limb was also normal.
Ultrasound KUB with bilateral renal artery Doppler was performed for which showed bilateral renal cortical cyst with renal parenchymal disease.
DIFFERENTIAL DIAGNOSIS:
Based on history, examination, labs and radiological findings, a diagnosis of Hypertension with left sided Polyneuritis cranialis secondary to an inflammatory pathology was made.
The differential diagnosis were kept as follow:
- Inflammatory diseases (atypical GBS, vasculitis)
- Infection (Herpes, VZV, Diphtheria, Lyme’s disease)
- Motor neuron disease (bulbar onset)
- Syringobulbia
- Neoplastic (Brainstem glioma )
- Bulbar Myasthenia Gravis
- Sarcoidosis
- Vascular (Brainstem stroke)
CSF ANALYSIS LEADING TO A DEFINITIVE DIAGNOSIS!
After taking a written informed consent, the lumbar puncture was performed and CSF was examined. Total of 10 cells were isolated with 80% lymphocytes. It showed albumin-cytological dissociation with micro albumin levels of 468.686 mg/dl.
FINAL DIAGNOSIS
Polyneuritis Cranialis – Atypical GBS.
TREATMENT
The patient was started on intravenous immunoglobulins at the dose of 2grams per kg over 5 days. After 4 days, patient started responding in the form of able to lift left arm overhead, relief in hoarseness of voice, able to swallow food bolus and lastly improvement in tongue deviation. He was also started on antihypertensive- calcium channel blocker and angiotensinogen converting enzyme inhibitor was discharged with advice to follow up in our clinic.