A case of Longitudinally Extensive Transverse Myelitis: Sarcoid Myelitis
Navneet Gupta1, Aarti Yadav1, Amrinder Singh2, Monika Tanwar3, Aanchal Arora4, Atul Goel5
https://meditropics.com/cr1-2022-2/
1Junior Resident,2Senior Resident, Department of Medicine, ABVIMS and RML Hospital, New Delhi
3Assistant Professor, Department of Medicine, ABVIMS and RML Hospital, New Delhi
4Assistant Professor, Department of Medicine, LHMC and RML Hospital, New Delhi
5Professor and Head of Unit, Department of Medicine, LHMC and RML Hospital, New Delhi
Abstract
Sarcoidosis primarily affects the lungs and lymphatic system but can affect any system including the central nervous system which is termed as Neurosarcoidosis. Central nervous system involvement presents with extremely variable findings which have overlap with other neurological diseases, thus making it a diagnostic challenge. Herein we present a case of 38-year-old female who presented with sub-acute onset upper motor neuron quadriparesis with asymmetric sensory and bowel bladder involvement. Lumbar puncture examination revealed cytoalbuminologic dissociation. Imaging showed longitudinally extensive transverse myelitis with dorsal subpial enhancement which pointed towards the diagnosis of Sarcoid Myelitis. Patient had gradual improvement in her symptoms after starting steroids and was discharged for outpatient follow-up.
Keyword: Neurosarcoidosis; Longitudinally Extensive Transverse Myelitis; Sarcoid myelitis
Introduction
Sarcoidosis is multi system inflammatory disorder characterized by presence of non-caseating granulomas in various parts of the body (1). The disease has a high geographical variability with northern European and African American populations reporting the highest incidence rates of 17-24 per 1, 00,000 populations (2). The lungs and the lymphatic system are the most commonly involved organs but the disease can involve virtually any organ and present with varied cardiac, neurological, ocular, kidney or laryngeal localizations (3). About 5% cases present with neurological manifestations hence termed neurosarcoidosis with more than half of patients presenting with isolated neurological syndrome as the first episode (4,5). Various clinical manifestations include cranial neuropathies, spinal cord inflammation, peripheral neuropathy or myopathy and chronic meningitis. Less than 10% cases of neurosarcoidosis present with spinal cord involvement termed as Sarcoid myelitis. Transverse myelitis presents as acute/subacute onset motor, sensory and autonomic spinal cord dysfunction (6). It has multiple causes broadly categorised into parainfectious, paraneoplastic, drug/toxin-induced, systemic autoimmune disorders and demyelinating diseases like multiple sclerosis (MS) or neuromyelitis optica (NMO). The diagnosis remains a diagnostic challenge since clinical, radiological and laboratory findings are non-specific and can be seen in a variety of neurological diseases. 15-30% cases are classified as idiopathic (7). Herein we report a case of longitudinally extensive transverse myelitis (LETM) presenting as subacute onset upper motor neuron symmetric quadriparesis as first manifestation of sarcoidosis.
Case Report
A 38year old lady presented to the emergency room of our hospital with complaints of generalized weakness for 20 days. The patient was apparently well 20 days back when she developed neck pain which was sharp shooting in character with radiation to back. This was associated with numbness and tingling in bilateral upper limbs. Following this the patient developed weakness of both upper limbs which progressed to involve bilateral lower limbs as well over the last 20 days. The patient was unable to sit up or roll in bed, had associated complaints of urinary retention and non-passage of stools over the last few days. There was no history of head trauma or fall. She denied history of fever, rash, diarrhoea, arthralgias or any other medical illness. There was no history of dry mouth, dry eyes, oral ulcers, hair loss or irregular menstrual cycles. She did not report any chronic cough or breathlessness. Weakness was not associated with loss of consciousness, headache, vomiting, convulsions or visual disturbances. There was no history suggestive of cranial nerve palsy.
On examination the patient was lying on bed, conscious oriented to time, place and person. Her blood pressure was 130/80 mm Hg, pulse was 120 per minute, oxygen saturation 97% on room air. Central nervous system examination revealed flaccidity in upper limbs with grade 0/5 power and normal tone in lower limbs with grade 3/5 power. All deep tendon reflexes were diminished and bilateral plantars were mute. There were reduced pain, touch, temperature sensations in both upper limbs while they were preserved elsewhere over the body. None of the cranial nerves were involved. There was no demarcated sensory level. Fundus examination was normal. Rest systemic examination was normal. Considering the presence of upper motor neuron quadriparesis with patchy sensory loss and bowel bladder involvement, a clinical diagnosis of myelitis with arachnoiditis with spinal shock was made. Possible etiologies could be post infectious or autoimmune disease, tuberculosis, neurosarcoidosis and multiple sclerosis.
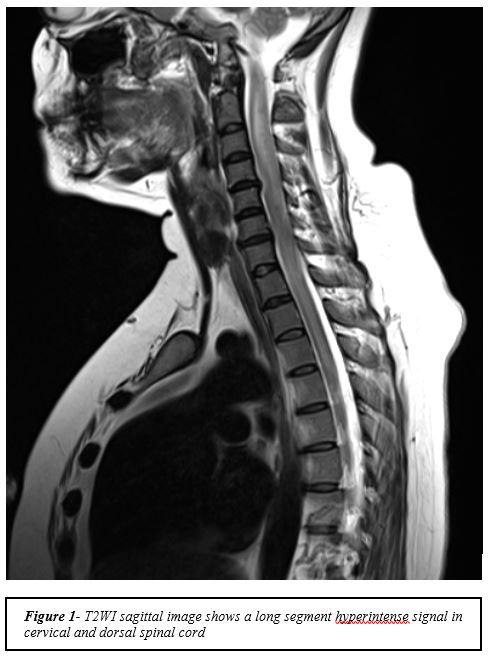
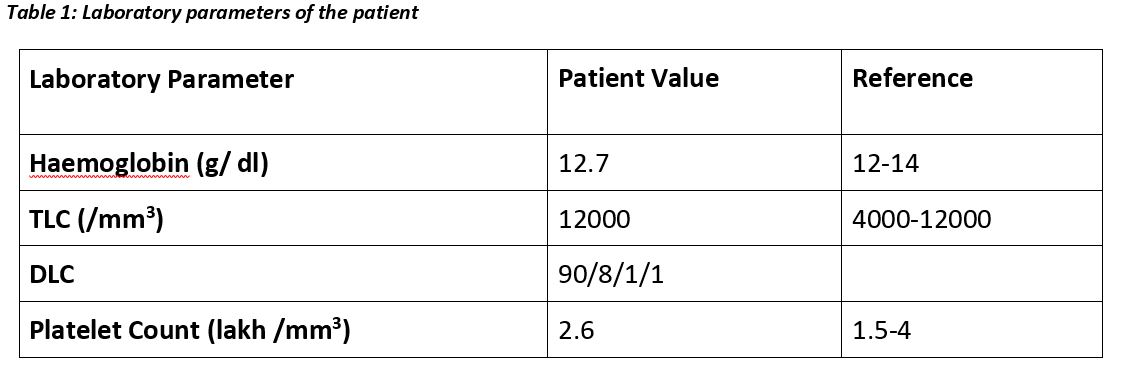
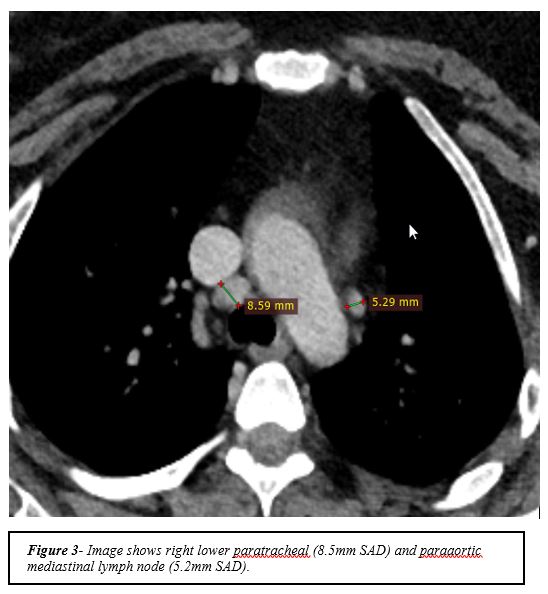
Routine investigations revealed normal haematological and biochemical parameters (Table 1). X ray spine and chest were also normal. Lumbar puncture was done which revealed raised opening pressure with evidence of cytoalbumin dissociation (2-3 mononuclear cells and 1.2 g/dl of protein, 54 mg/dl glucose). Considering the above possible differentials other investigations such as Antinuclear Antibody (ANA), Extractable Nuclear Antigens (ENA), Antiphospholipid antibody (APLA), Cerebrospinal fluid (CSF) gram stain and culture, CSF CBNAAT for tuberculosis (TB), CSF TB PCR, Mantoux, HIV, HBsAg, anti-HCV, EBV serology and TORCH serology were all negative (Table 1). Serum Angiotensin Convertase Enzyme (ACE) levels were normal. Magnetic Resonance Imaging (MRI) spine was done which revealed extensive long segment central intramedullary signal alteration in cervical, thoracic and lumbar segment with abnormal dorsal subpial contrast enhancement likely due to neurosarcoidosis (Figure 1). Computed tomography (CT) chest was done which revealed multiple homogenously enhancing subcentimetric discrete lymph nodes in mediastinum at paratracheal, subcarinal and right hilar region (Figure 2); well-defined hypoenhancing soft tissue lesion in anterior mediastinum likely thymic hyperplasia.
On basis of imaging evidence, a diagnosis of neurosarcoidosis was made and patient was started on pulse injection methyl prednisone for 5 days. The patient had gradual improvement in her weakness and became ambulatory a week following the last dose of pulse steroid. Bladder and bowel control was also regained. Repeat lumbar puncture done after two weeks revealed elevated pressure, acellular cytology, 113 mg/dl protein and 50 mg/dl glucose. After two weeks of admission the patient was discharged on maintenance dose (1mg/kg body weight) of steroid to follow up in outpatient clinic after two weeks. On follow up, she had complete neurological recovery and was started on oral azathioprine 50 mg once a day with tapering doses of oral steroid. Since then the patient is doing well.
Investigations
Discussion
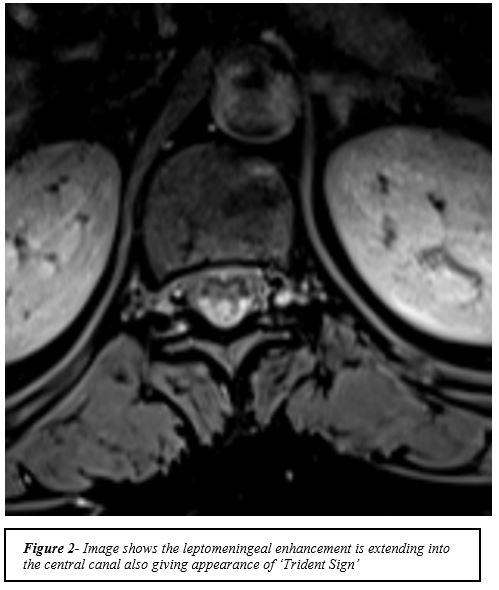
Neurosarcoidosis presents with spinal cord dysfunction in less than 10% of the cases. The disease tends to present with longitudinally extensive lesions generally involving 3 or more segments with thoracic segment most commonly affected followed by cervical segment. Common clinical presentations include lower extremity weakness and paraesthesia (8). Laboratory findings include raised C reactive protein (CRP), Lactate dehydrogenase (LDH) and hyper-gamma globulinemia (9). CSF examination typically reveals pleocytosis along with raised protein and oligo-clonal bands in about 20-30 % of the samples (9). Common MRI findings include longitudinally extensive myelitis with associated dorsal or ventral subpial enhancement, short tumefactive myelitis, spinal meningitis/meningo radiculitis and anterior myelitis (10). Among the above lesions longitudinally extensive myelitis is the most common lesion (10). Dorsal subpial enhancement leads to the formation of trident sign (Figure 3) which can serve as an important differentiating feature from NMO spectrum disorder(11,12).
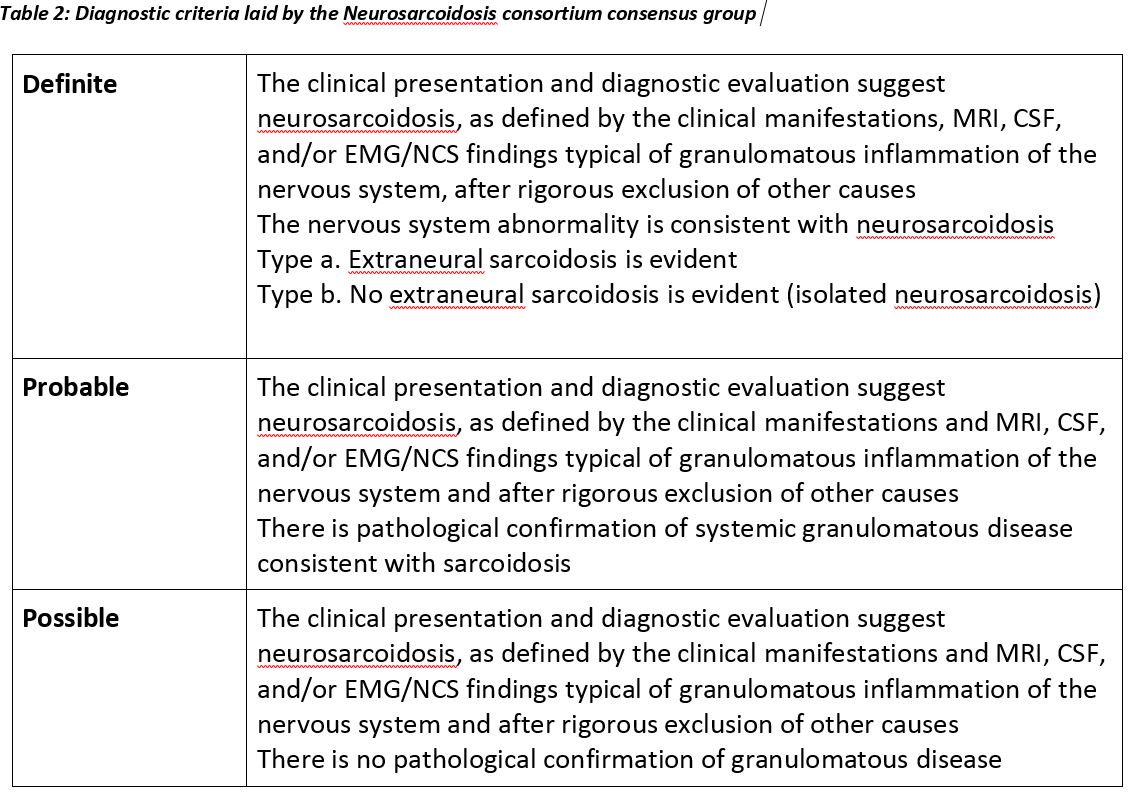
The disease is diagnosed as definite, probable or possible as per the diagnostic criteria laid by the Neurosarcoidosis consortium consensus group [Table 2](13).
Treatment options include initial treatment with high dose glucocorticoids followed by switching on to maintenance therapy and addition of a Disease Modifying Anti – Rheumatic Dug (DMARD). Our patient had presented with quadriparesis with bowel bladder involvement with sensory loss in upper limbs. On the basis of history, examination and imaging of the spine a diagnosis of LETM was kept. Further on the basis of spinal cord lesions, CT chest findings and exclusion of other possible causes of LETM a diagnosis of possible Sarcoid Myelitis was made. The patient had complete recovery and is currently on follow up in our outpatient department.
References
- Statement on Sarcoidosis. Am J Respir Crit Care Med. 1999 Aug 1;160(2):736–55.
- Gerke AK, Judson MA, Cozier YC, Culver DA, Koth LL. Disease Burden and Variability in Sarcoidosis. Ann Am Thorac Soc. 2017 Dec;14 (Supplement_6):S421–8.
- Nunes H, Bouvry D, Soler P, Valeyre D. Sarcoidosis. Orphanet J Rare Dis. 2007 Nov 19;2:46.
- Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H, Bresnitz EA et al. Clinical Characteristics of Patients in a Case Control Study of Sarcoidosis. Am J Respir Crit Care Med. 2001 Nov 15;164(10):1885–9.
- Fritz D, van de Beek D, Brouwer MC. Clinical features, treatment and outcome in neurosarcoidosis: systematic review and meta-analysis. BMC Neurol. 2016 Nov 15;16(1):220.
- Frohman EM, Wingerchuk DM. Clinical practice. Transverse myelitis. N Engl J Med. 2010 Aug;363(6):564–72.
- de Seze J, Stojkovic T, Breteau G, Lucas C, Michon-Pasturel U, Gauvrit JY, et al. Acute myelopathies: Clinical, laboratory and outcome profiles in 79 cases. Brain. 2001 Aug;124(Pt 8):1509–21.
- 8. Sohn M, Culver DA, Judson MA, Scott TF, Tavee J, Nozaki K. Spinal cord neurosarcoidosis. Am J Med Sci. 2014 Mar;347(3):195–8.
- Cohen-Aubart F, Galanaud D, Grabli D, Haroche J, Amoura Z, Chapelon-Abric C, et al. Spinal cord sarcoidosis: clinical and laboratory profile and outcome of 31 patients in a case-control study. Medicine (Baltimore). 2010 Mar;89(2):133–40.
- Murphy OC, Salazar-Camelo A, Jimenez JA, Barreras P, Reyes MI, Garcia MA, et al. Clinical and MRI phenotypes of sarcoidosis-associated myelopathy. Neurol – Neuroimmunol Neuroinflammation. 2020 Jul 2;7(4):e722.
- Zalewski NL, Krecke KN, Weinshenker BG, Aksamit AJ, Conway BL, McKeon A, et al. Central canal enhancement and the trident sign in spinal cord sarcoidosis. Neurology. 2016 Aug 16;87(7):743 LP – 744.
- Jolliffe EA, Keegan BM, Flanagan EP. Trident sign trumps Aquaporin-4-IgG ELISA in diagnostic value in a case of longitudinally extensive transverse myelitis. Mult Scler Relat Disord. 2018 Jul;23:7–8.
- Stern BJ, Royal W 3rd, Gelfand JM, Clifford DB, Tavee J, Pawate S, et al. Definition and Consensus Diagnostic Criteria for Neurosarcoidosis: From the Neurosarcoidosis Consortium Consensus Group. JAMA Neurol. 2018 Dec;75(12):1546–53.