Preventive measures for avoiding post transfusion reactions and mismatch
https://meditropics.com/660-2/
Sourav Kumar
Post graduate resident, Department of Medicine, LHMC
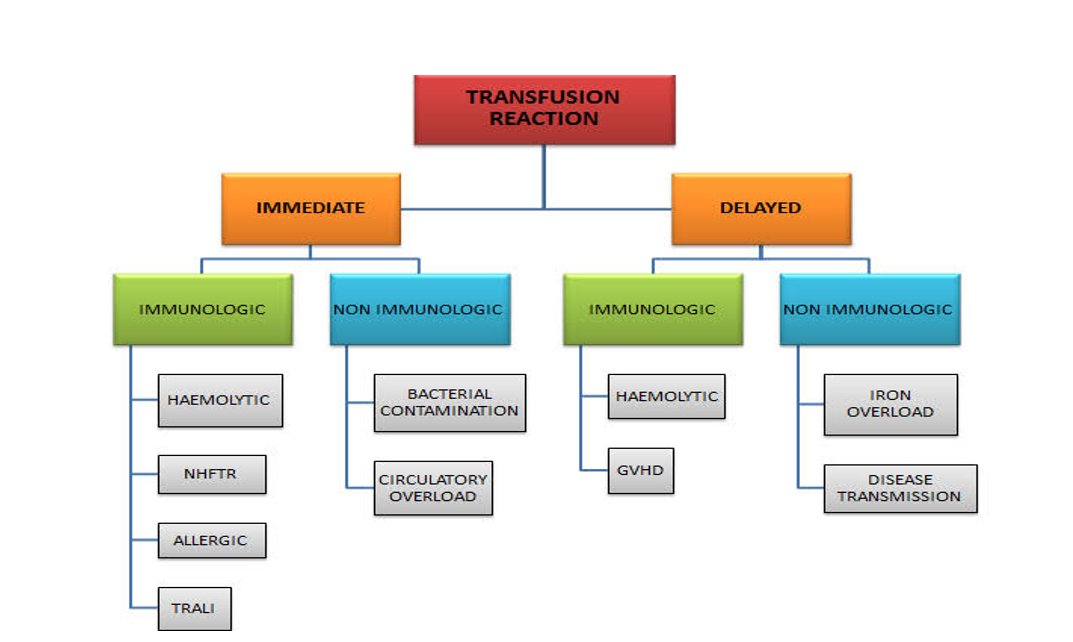
The most common complications of transfusion are
(a)Febrile reactions
(b)Chill-rigor reactions
The most serious complications, which have very high mortality rates, are
1)Acute hemolytic reaction (AHTR) due to ABO incompatibility
2)Graft-vs-host disease (GVHD)
3)Transfusion-associated circulatory overload (TACO)
4)Transfusion-related acute lung injury (TRALI)
Other complications include
- Allergic reactions
- Altered oxygen affinity
- Delayed hemolytic transfusion reaction
- Infections
- Post-transfusion purpura
- Iron overload
Febrile reactions
Cause-
- Antibodies directed against white blood cell human leukocyte antigen (WBC HLA) in otherwise compatible donor blood
- Cytokines released from WBCs during storage, particularly in platelet concentrates
Prevention
- special leukoreduction filters are used during transfusions;
- leukoreduced (WBC-depleted RBCs) blood components.
Acute hemolytic transfusion reactions
ABO incompatibility is the most common cause of acute hemolytic transfusion reaction. Antibodies against blood group antigens other than ABO can also cause AHTR.
Mislabeling the recipient’s pretransfusion sample at collection and failing to match the intended recipient with the blood product immediately before transfusion are the usual causes.So avoid these errors.
Graft vs host disease
caused by transfusion of products containing immunocompetent lymphocytes to an immunocompromised host .The donor lymphocytes attack host tissues because the host immune system cannot destroy donor lymphocytes. Graft-vs-host disease can occur occasionally in immunocompetent patients if they receive blood from a donor (usually a close relative) who is homozygous for an human leukocyte antigen (HLA) haplotype for which they are heterozygous.
Prevention of graft-vs-host disease is with irradiation (to damage DNA of the donor lymphocytes) of all transfused blood products. It is done:-
- When the recipient is immunocompromised (eg, patients with congenital immune deficiency syndromes, hematologic cancers, or hematopoietic stem cell transplants; neonates)
- When donor blood is obtained from a 1st-degree relative
- When HLA-matched components, excluding stem cells, are transfused
Transfusion associated circulatory overload(TACO)
Cause:-The high osmotic load of blood products draws volume into the intravascular space over the course of hours, which can cause transfusion-associated circulatory overload in susceptible patients (eg, those with cardiac or renal insufficiency).
Prevention:-RBCs should be infused slowly. The patient should be observed and, if signs of heart failure (eg, dyspnea, crackles) occur, the transfusion should be stopped and treatment for heart failure begun.Typical treatment is with a diuretic such as furosemide 20 to 40 mg IV or better way is to give furosemide 20 mg IV in middle of transfusion .
Transfusion-related acute lung injury (TRALI):-
Cause:-Transfusion-related acute lung injury is an infrequent complication caused by anti-HLA and/or anti granulocyte antibodies in donor plasma that agglutinate and degranulate recipient granulocytes within the lung.Acute respiratory symptoms develop within 6 hours , and chest x-ray has a characteristic pattern of noncardiogenic pulmonary edema.
Prevention:-
1)screening of all donors for anti-HLA Or anti neutrophilic antibodies
2) Using leuko-reduced blood
Allergic reactions:-
Allergic reactions to an unknown component in donor blood are common, usually due to allergens in donor plasma or, less often, to antibodies from an allergic donor. These reactions are usually mild and include urticaria, edema, occasional dizziness, and headache during or immediately after the transfusion.
Prevention:-
In a patient with a history of allergies or an allergic transfusion reaction, an antihistamine may be given prophylactically just before or at the beginning of the transfusion (eg, diphenhydramine 50 mg orally or IV).
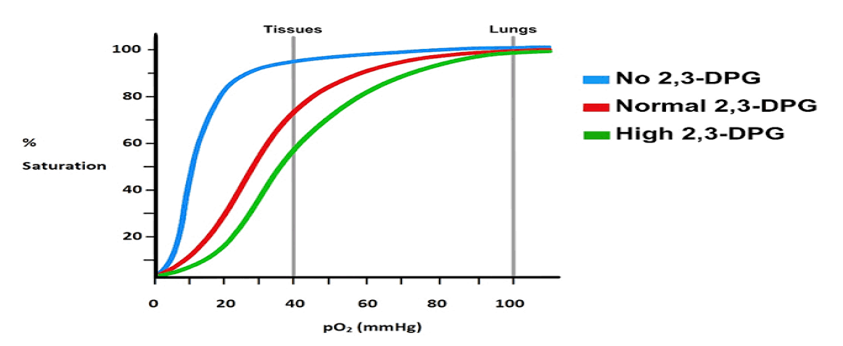
Altered oxygen affinity:-
Blood stored for > 7 days has decreased RBC 2,3-diphosphoglycerate (DPG), and the 2,3-DPG is absent after >10 days. This absence results in an increased affinity for oxygen and slower release of oxygen to the tissues. After transfusion of RBCs, 2,3-DPG regenerates within 12 to 24 hours.
Delayed hemolytic transfusion reaction:-
In some people there may be cross reactivity between Rh, duffy, kidd, kell antigen and antibodies against it, this may result in an anamnestic response which usually occur after 24 hours to 1 week and cause a delayed hemolytic transfusion reaction. Usually, only hemolysis of the transfused RBCs occurs which contains antigen against which specific non detectable level of IgG antibodies are already there in recipient body formed in past exposure, this results in a falling hematocrit and a slight rise in lactate dehydrogenase and bilirubin and a positive direct antiglobulin test. Because delayed hemolytic transfusion reaction is usually mild and self-limited, it is often unidentified and just require conservative management.
Infectious complications
- Bacterial contamination of packed RBCs occurs rarely, possibly due to inadequate aseptic technique during collection or due to transient asymptomatic donor bacteremia. Refrigeration of RBCs usually limits bacterial growth except for cryophilic organisms such as Yersinia, which may produce dangerous levels of endotoxin.
- To minimize growth, storage is limited to 5 days. All RBC units are inspected before dispensing for bacterial growth, which is indicated by a color change. Rarely, syphilis is transmitted in fresh blood or platelets. Storing blood for ≥ 96 hours at 4 to 10° C kills this spirochete.
- Hepatitis may occur after transfusion of any blood product. The risk has been reduced by viral inactivation through heat treatment of serum albumin and plasma proteins and by the use of recombinant factor concentrates. Tests for hepatitis are compulsory for all donor blood
- For HIV, Testing for antibodies to both strains are required. Nucleic acid testing for HIV-1 antigen and HIV-1 p24 antigen testing are also required. Additionally, blood donors are asked about behaviours that may put them at high risk of HIV infection.
- Cytomegalovirus (CMV) can be transmitted by WBCs in transfused blood. It is not transmitted through fresh frozen plasma. Because CMV does not cause disease in immunocompetent recipients, routine antibody testing of donor blood is not required. However, CMV may cause serious or fatal disease in immunocompromised patients, who should receive blood products that are CMV-negative by antibody testing or blood depleted of WBCs by filtration.
- Malaria is transmitted easily through infected RBCs. Storage does not render blood safe. Prospective donors must be asked about malaria or whether they have been in a region where it is prevalent. Donors who have had a diagnosis of malaria or who are immigrants, refugees, or citizens from countries in which malaria is considered endemic are deferred for 3 years; travellers to endemic countries are deferred for 1 year.
- Hypothermia due to rapid transfusion of large amounts of cold blood can cause arrhythmias or cardiac arrest. Hypothermia is avoided by using an IV set with a heat-exchange device that gently warms blood.
Electrolyte abnormalities: –
Citrate and potassium toxicities generally are not of concern even in massive transfusion; however, toxicities of both may be amplified in the presence of hypothermia. Patients with liver failure may have difficulty metabolizing citrate. Hypocalcaemia can result but rarely necessitates treatment (which is 10 mL of a 10% solution of calcium gluconate IV diluted in 100 mL D5W, given over 10 minutes). Patients with kidney failure may have elevated potassium if transfused with blood stored for > 1 week (potassium accumulation is usually insignificant in blood stored for < 1 week). Mechanical haemolysis during transfusion may increase potassium. Hypokalaemia may occur about 24 hours after transfusion of older RBCs (> 3 weeks), which take up potassium.
Transfusion related iron overload: –
Transfusion iron overload is directly associated with the number of blood transfusions. One unit of transfused blood contains about 200-250 mg of iron. In general, patients who receive more than 10 to 20 units of blood are at a significant risk of iron overload. Patients who become transfusion dependent with thalassemia, myelodysplastic syndrome, sickle cell anemia, aplastic anemia, hemolytic anemia, etc. inevitably develop iron overload.
Prevention: –Prophylactic iron chelation therapy should be initiated before clinically significant iron overload occurs. Deferoxamine and deferasirox are commonly used.
References
1.Ezidiegwu CN, Lauenstein KJ, Rosales LG, Kelly KC, Henry JB. Febrile nonhemolytic transfusion reactions. Management by premedication and cost implications in adult patients. Arch Pathol Lab Med. 2004 Sep;128(9):991-5. doi: 10.5858/2004-128-991-FNTR.
2.Duran J, Siddique S, Cleary M. Effects of Leukoreduction and Premedication With Acetaminophen and Diphenhydramine in Minimizing Febrile Nonhemolytic Transfusion Reactions and Allergic Transfusion Reactions During and After Blood Product Administration: A Literature Review With Recommendations for Practice. J Pediatr Oncol Nurs. 2014 Jul;31(4):223-229.
3.Sanders RP, Maddirala SD, Geiger TL, Pounds S, Sandlund JT, Ribeiro RC, Pui CH, Howard SC. Premedication with acetaminophen or diphenhydramine for transfusion with leucoreduced blood products in children. Br J Haematol. 2005 Sep;130(5):781-7. doi: 10.1111/j.1365-2141.2005.05670.
4.National AIDS Control organisation guidelines 2021.
5.Frazier SK, Higgins J, Bugajski A, Jones AR, Brown MR. Adverse Reactions to Transfusion of Blood Products and Best Practices for Prevention. Crit Care Nurs Clin North Am. 2017 Sep;29(3):271-290. doi: 10.1016/j.cnc.2017.04.002. Epub 2017 Jun 26.