Cutaneous vasculitis in systemic lupus erythematosus: Clinical vignette
Authors
Rajat Kharbanda1, Harshita Umesh2, Latika Gupta1
Affiliation
1 Department Clinical Immunology and Rheumatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
2 Bangalore Medical College and Research Institute, Bangalore, Karnataka, India
Address for correspondence
Dr Latika Gupta
Assistant Professor
Department of Clinical Immunology and Rheumatology
Sanjay Gandhi Postgraduate Institute of Medical Sciences
Lucknow, India
Email: drlatikagupta@gmail.com
Phone number: 05222495182
Running title: Rashes in SLE
Funding statement: No funding was received.
Competing interest: The authors declare that they have no competing interests.
Disclosures: The authors have nothing to disclose.
Contribution: All authors were involved in manuscript ideation and preparation.
Acknowledgements: None
https://meditropics.com/pgr1-2022-2/
Abstract.
Purpuric rashes on the palms and soles in a patient with systemic lupus erythematosus (SLE) can be attributed to vasculitis, catastrophic anti-phospholipid syndrome (CAPS), or thrombotic thrombocytopenic purpura (TTP). It is difficult to differentiate between these conditions due to overlapping clinical presentation, and a high index of suspicion may help with timely diagnosis and management. Herein we report the case of a 27-year-old lady presenting with SLE related multisystem involvement and a blanchable purpuric rash, which was managed with immunosuppressive agents.
Keywords. systemic lupus erythematosus, vasculitis, catastrophic anti-phospholipid syndrome, thrombotic thrombocytopenic purpura
Case.
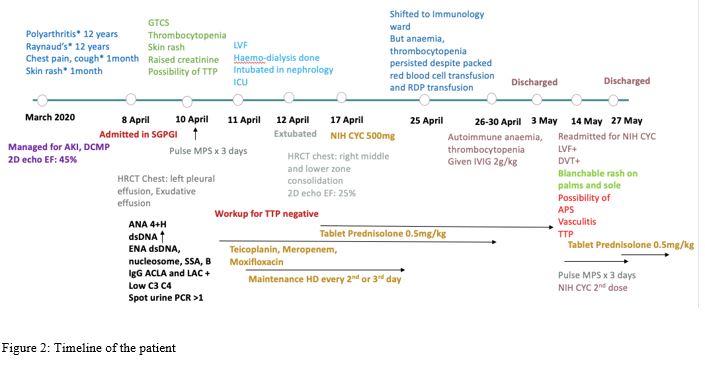
A 27-year-old lady presented to the rheumatology department with inflammatory polyarthritis of the hand joints and raynaud’s of 12 years duration. At presentation, she seemed to have myocarditis since the past one month, along with petechial rashes (over dependant areas), generalised tonic-clonic seizures and oliguria. She also reported a bad obstetric history with spontaneous pregnancy loss at 8 weeks period of gestation. On physical examination, she was hypertensive and tachycardia was evident, and she required 2 litres O2 per minute to maintain saturation. Palpable purpura was present over the entire back and extremities, and coarse crepitations and decreased breath sounds were noted in the left mammary, infra-axillary, infra-scapular areas. Cardiac examination showed right parasternal loud and loud P2 on auscultation.
With these findings, possibility of myocarditis with congestive cardiac failure was considered alongside seizure disorder, arthritis, and ongoing vasculitis. The rashes could also be attributed to thrombocytopenic purpura, or thrombosis which could both be seen in systemic lupus erythematosus. Investigation revealed anaemia (5.2 g%), absence of schistocytes in peripheral smear with elevated lactate dehydrogenase (761 U/L), thrombocytopenia (64000/mm3, lymphopenia, raised serum creatinine (3.7 mg/dl). Lupus was confirmed by the autoantibody profile–positive anti-nuclear antibody (4+homogenous), raised dsDNA, nucleosome and SS-A antibodies. She had moderately high titres (40 GPL) of IgG Ig G antiphospholipid anticardiolipin antibody (ACLA) with titres of 40 GPL, while beta-2 glycoprotein 1 and Ig M ACLA were negative. She also tested positive for Lupus anticoagulant. Complements were low (C3: 38mg/dl C4: 18mg/dl). Urinalysis showed bland proteinuria without active urine sediment and urine protein creatinine ratio of >1. Thoracic Computed tomography (CT) revealed massive left sided pleural effusion, which was transudative. CT head was normal. 2D echo had reduced LV contractility with global hypokinesia with LVEF of 25%.
Thus, a diagnosis of SLE was confirmed with major organ involvement (renal, cardiac, neurological). She was treated with methylprednisolone pulse (750mg/day for 3 days) followed by oral prednisolone by 1mg/kg, hemodialysis for acute kidney injury. and cyclophosphamide (CYC) 500mg. With persistent autoimmune cytopenias, intravenous immunologlobulin (2g/kg) was given with notable improvement over the next two weeks. Despite intense immunosuppression she developed deep vein thrombosis (DVT) involving right femoral vein and proximal saphenofemoral vein. and subsequently rash over palms and soles (Figure 1A, B). At this juncture the three possibilities included small vessel vasculitis, catastrophic phospholipid syndrome (CAPS) and thrombotic thrombocytopenic purpura (TTP) were kept. The first one may be occasionally associated with thrombosis, while the other two are inevitably associated with thrombocytopenia.
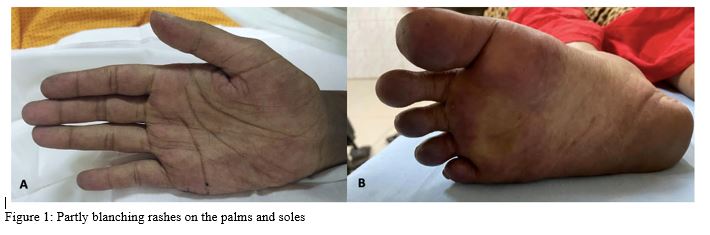
Peripheral smear did not suggest schistocytes, and LDH was normal, essentially ruling out TTP. CAPS is a rare but life threating emergency, which often is difficult to diagnose and establish histopathologically. Since the rashes on palms were partly blanching, and seemed to involve the small vessels, active ongoing vasculitis seemed more likely on a background of severe lupus with major organ involvement. Thus, further pulse methylprednisolone 500mg was administered for 2 days following which rash progression halted. With clinical (DVT) and serological findings of APS, anticoagulation with LMWH was initiated and oral steroids in a dose of 1mg/kg prednisolone were continued (Figure 2)
Discussion.
This patient presented with multi-organ dysfunction with involvement of hematological, renal, cardiovascular, respiratory and renal system. SLE vasculitis can have diverse clinical presentation with involvement of small, medium or large vessels, though cutaneous manifestation being commonest, points towards small vessel vasculitis.[1] Symptoms can be non-specific and overlap with features of APS and TTP. [2] The presence of thrombocytopenia with rashes may be salient pointers to other sinister aetiologies (such as TTP and CAPS) lurking in the background in active lupus. A keen eye of suspicion is vital to establish these as treatment may differ and timely management can be lifesaving.
References.
- Golan, T.D. Lupus vasculitis: Differential diagnosis with antiphospholipid syndrome. Curr Rheumatol Rep4, 18 (2002). https://doi.org/10.1007/s11926-002-0019-8
- Barile-Fabris L, Hernández-Cabrera MF, Barragan-Garfias JA. Vasculitis in systemic lupus erythematosus. Curr Rheumatol Rep. 2014;16(9):440. doi:10.1007/s11926-014-0440-9