https://meditropics.com/lipid-disorder-and-pcks9-inhibitors-a-short-review/
*Lohani KK, **Sundarka MK *Professor & Head, Medicine, NSMCH, Bihta, Patna, **Honorary Consultant Physician, BG Clinic, Delhi.
Abstract
Dyslipidemia is a major contributor to morbidity and mortality, and it stands as the most prevalent risk factor for cardiovascular disease (CVD). The management of dyslipidemia has traditionally involved targeting various enzymatic processes in cholesterol metabolism. Among these processes, targeting hepatocytes released enzyme called PCSK9 (Proprotein Convertase Subtilisin/Kexin type 9), which leads to the degradation of LDL-receptors and results in elevated blood LDL-C levels, is stirring. Inhibiting this enzyme, typically through monoclonal antibodies (mAb), facilitates the recycling of LDL-receptors and consequently lowers blood LDL-C levels. This gave rise to the concept of PCSK9 Inhibitors, which are administered through subcutaneous injection. However, despite their significant effectiveness in reducing LDL-C, these inhibitors are not widely employed in routine clinical practice. This limited use can be attributed to factors such as cost and the need for subcutaneous injection. As a result, statins continue to be the primary treatment for dyslipidemia due to their safety record, cost-effectiveness, and substantial supporting evidence. PCSK9 Inhibitors are considered supplementary treatments to be used in conjunction with statins. Lifestyle modifications play an essential role in managing dyslipidemia.
Key words: PCSK9 Inhibitor, Statin, Dyslipidemia, LDL-C, PCSK9i
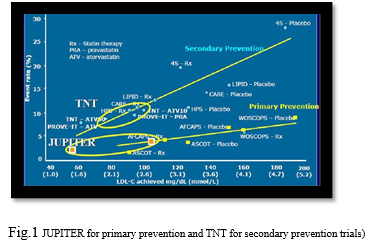
This short review is focused on PSCK-9 inhibitors. Dyslipidemia is a significant contributor to morbidity and mortality and is recognized as the most common risk factor for cardiovascular disease (CVD), as indicated by the global INTERHEART study. Dyslipidemia management is guided by evolving international guidelines, with a consistent focus on LDL-C as the primary treatment target. Lowering LDL-C levels has been established as an effective approach in both primary and secondary prevention, as demonstrated in trials like JUPITER and TNT (1) [Fig1].
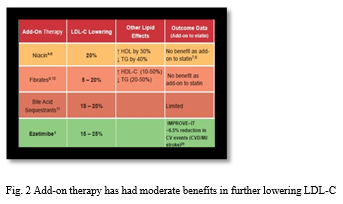
Statins have been the cornerstone of LDL-C reduction for nearly two decades, with moderate- intensity statins typically used initially and dose adjustment as needed. Statins are the foundation of the prevention and treatment of atherosclerotic cardiovascular disease (ASCVD). Nevertheless, even at maximum statin therapy, some patients do not achieve their target LDL-C levels, necessitating additional treatment options. Add-on therapy has had moderate benefits in further lowering LDL-C as shown in Fig. 2 . Therefore, there has been an unmet clinical need for novel lipid-lowering agents that can target low-density lipoprotein cholesterol (LDL-C) and other atherogenic particles (2).
For all practical purposes, currently, only two main modalities are available for reducing LDL-C: statins, which inhibit the HMG-CoA reductase enzyme, and Ezetimibe, a drug that reduces cholesterol absorption in the small intestine.
Recently, developed oral add-on drug Bempedoic acid, which inhibits LDL-C synthesis in the liver, is also as potent as Ezetimibe. Bempedoic acid is an adenosine triphosphate citrate lyase (ACL) inhibitor which inhibits cholesterol synthesis in the liver, thereby lowering LDL-Cholesterol (3). Thus, there is a definite need for another modality of treatment that can further reduce LDL-C levels in high and very high-risk patients (4). During the past decade, several drugs have been developed for the treatment of dyslipidemia (2).
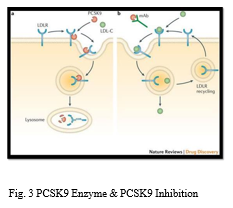
PCSK9 Enzyme: The breakthrough discovery of proprotein convertase subtilisin/kexin type 9 (PCSK9) 20 years ago revolutionized the current understanding of cholesterol homeostasis. Genetic studies have shown that gain-of-function mutations in PCSK9 lead to elevated LDL cholesterol and increased risk of atherosclerotic cardiovascular disease, while loss-of-function mutations in PCSK9 result in lifelong low levels of circulating LDL cholesterol and dramatic reduction in atherosclerotic cardiovascular disease (5). The clearance of LDL cholesterol from the bloodstream relies on hepatic LDL receptors. LDL binds to LDL receptors (LDLR) on the surface of liver cells, undergoes endocytosis, and is transported to lysosomes for degradation. LDL receptors are then recycled to the cell surface to bind to LDL again, contributing to LDL removal from plasma. However, hepatic cells secrete PCSK9, an enzyme that causes LDL- receptor degradation and leads to elevated blood LDL-C levels. Inhibition of PCSK9, typically through monoclonal antibodies (mAb), ensures LDL-receptor recycling and a subsequent reduction in LDL-C levels, giving rise to the concept of PCSK9 Inhibitors (6) [Fig 3].
PCSK9 Inhibitors: PCSK9 inhibition can result in a substantial 60% reduction in LDL-C, as demonstrated in trials like Fourier. There are three PCSK9 inhibitors currently available, all in the form of monoclonal antibodies for subcutaneous injection. They bind to a pro-protein involved in the regulation of LDL receptors on liver cells; receptor numbers are increased, which results in increased uptake of LDL-cholesterol from the blood (3).
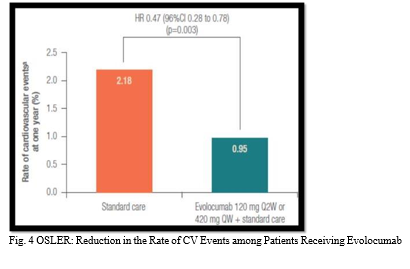
Evolocumab (marketed by Amgen) – OSLER Trial (Fig4).
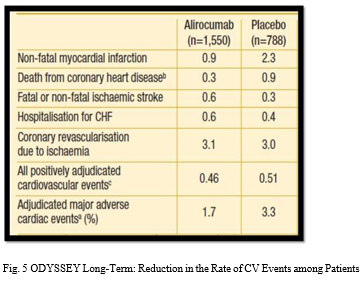
Alirocumab (marketed by Sanofi) – ODYSSEY Trial (Fig 5). Bococizumab (expected release by Pfizer) – SPIRE trial
The SPIRE trial program, which was discontinued due to inadequate results related to anti-drug antibody formation.
The GLAGOV Study Investigated 970 patients with angiographic CAD over 78 weeks of treatment (LDL-C ≥ 2.07 mmol/L). The PCSK9 Inhibitors were associated with a reduction in atheroma volume on angiography (primary outcome) with more individuals demonstrating plague regression (64.3% vs. 47.3%). Fewer developed major adverse cardiac events (12.2% vs. 15.3%) compared to controls (secondary outcome) (7,8).
PCSK9 inhibitors appear to be well tolerated. The overall incidence of adverse events was similar with Alirocumab and Evolocumab vs. placebo. Based on current guidelines, available evidence, and economic considerations, patients with familial hypercholesterolemia (FH) or atherosclerotic cardiovascular disease (ASCVD) and statin resistance (on max dose) for additional LDL lowering is a reasonable strategy. It is second line with the addition of ezetimibe for statin-intolerant patients (NLA expert panel 2017).
Clinical trials have shown that Alirocumab and Evolocumab effectively lower LDL-C levels by around 60%, whether used alone or in combination with statins and/or ezetimibe, without any safety issues (9, 10).Its worth to mention few more new drugs which works differently and have a role in managing lipid disorders. Furthermore, several novel strategies to target PCSK9 are in development, including oral antibody, gene silencing, DNA base editing and vaccine therapies (5).
Another extremely effective lipid-lowering medication which is interfering with PCSK9 enzyme is Inclisiran. It’s a recent drug, which blocks PCSK9 mRNA. Inclisiran is a small interfering RNA which limits production of PCSK9, increasing uptake of LDL-cholesterol and thereby lowering levels in blood (3). This is indicated in cases of primary hypercholesterolemia or mixed dyslipidemia in combination with a statin, or with a statin and other lipid-lowering therapies, or with other lipid-lowering therapies or alone if a statin contra-indicated or not tolerated (3).
ApoA1 mimetic peptide is considered as a potential treatment to exploit the athero-protective effects of HDL-C, but needs more supporting evidences. We hope that these novel lipid-lowering agents can be used in real clinical settings in the near future (2).
Lomitapide, an inhibitor of microsomal triglyceride transfer protein (MTP), reduces lipoprotein secretion and circulating concentrations of lipoprotein-borne lipids such as cholesterol and triglycerides (3).
Volanesorsen is an antisense oligonucleotide which inhibits the formation of the Apo lipoprotein apoC–III, thereby lowering serum triglycerides. It is given as subcutaneous injection, indicated in familial chylomicronaemia syndrome for specialist use only (3).
CONCLUSION
The PCSK9 Inhibitors study has added confirmatory evidence to the LDL-C hypothesis. No doubt statins will be the frontline treatment for many years to come because of safety data, cost, and wealth of evidence. PCSK9i will remain an add-on to statin treatment. Despite the fact that PCSK9i abs significantly lower LDL-C, which is an effective way to lessen the burden of ASCVD, they are still not frequently utilized in routine clinical practice. In fact, they are only regarded as cost-effective in individuals with a very high risk of ASCVD, given an average annual cost of
$5400–$5800 (US dollars, year 2020 values) per patient. In spite of their acceptable tolerability, registry-derived adherence results are disappointing, reporting a discontinuation rate of 35– 40% after six months. This is likely due to the requirement for subcutaneous injection, which may decrease patient adherence. Another extremely effective lipid-lowering medication is the recently created Inclisiran, which blocks PCSK9 mRNA. Subcutaneous injections are also used, but they are far less in number. Last but not least, life style modification remains indispensable in the management of dyslipidemia (11).
Learning bites:
Statins continue to be the main treatment in lipid disorders due to their safety record, low cost, and substantial supporting evidence.
PCSK9 inhibition can result in a substantial 60% reduction in LDL-C, cost and non-oral form is a limiting factor.
Life style modification remains indispensable in the management of dyslipidemia.
References:
- Seidah Proprotein Convertase Subtilisin Kexin 9 (PCSK9) Inhibitors in the Treatment of Hypercholesterolemia and other Pathologies. Current Pharmaceutical Design. 2013 Apr 1; 19(17):3161– 72.
- Kim K, Ginsberg HN, Choi New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins. Diabetes & Metabolism Journal. 2022 Jul 31; 46(4):517–32.
- BNF is only available in the UK [Internet]. [cited 2023 Nov 5]. Available from: https://bnf.nice.org.uk/drugs/.
- Seidah NG, Awan Z, Chrétien M, Mbikay PCSK9: a key modulator of cardiovascular health. Circulationresearch[Internet].2014;114(6):1022 36.from: https://www.ncbi.nlm.nih.gov/pubmed/24625727
- Rishi Rikhi, Shapiro Proprotein Convertase Subtilisin/Kexin Type 9 Inhibition: The Big Step Forward in Lipid Control. European cardiology. 2023 Jun 28; 18.
- Emma PCSK9 inhibitors. The next cholesterol lowering blockbusters? The Pharmaceutical Journal. 2015; 294:7858
- Manoria PC al. PCSK9 Inhibitors: Potential as Fututre Lipid-Lowering Agents! Medicine Update 2016, Vol 2, API, Page 599-604.
- Nicholls SJ. Puri R, Aderson T, Ballantyne CM, Cho L, Kastelein JJ, et. al. Effect of Evolocumab on progression of Coronary Disease in statin-treated patients: The GLAGOV Randomized Clinical Trial. 2017 Nov 15 15.
- Stoekenbroek RM, Kallend D, Wijngaard PL, Kastelein JJ. Inclisiran for the treatment of cardiovascular disease: the ORION clinical development Fut Cardiol. 2018; 14(6):433–42.
- Kaufman TM, al. Application of PCSK9 Inhibitors in practice. Circ Res. 2019 Jan 04; 124(1), 32-37
- Azari S, et al. Cost-effectiveness analysis of PCSK9 inhibitors in cardiovascular diseases: a systematic Heart Fail Rev. 2020; 25(6):1077–88.