https://meditropics.com/babinski-sign/
*Sundarka M.K. MD, MRCP UK, DCN UCL, SCNeuro Fed RCP UK
*Consultant Physician & Neurologist, BG Clinic, New Delhi & Primary Care Specialist, NHS, England.
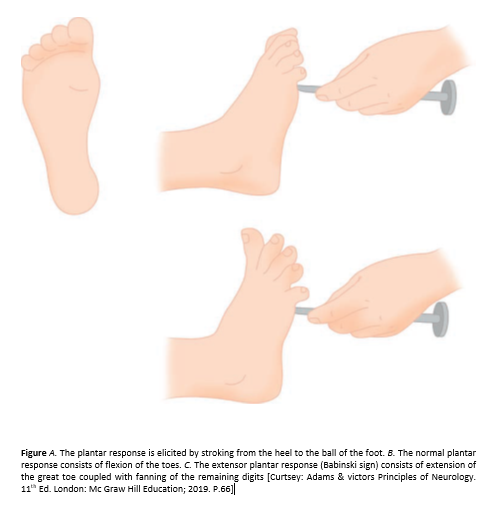
Stroking the lateral part of the sole of the foot with a fairly sharp object produces plantar flexion of the big toe; often there is also flexion and adduction of the other toes. This normal response is termed the flexor plantar reflex. In some patients, stroking the sole produces extension (dorsiflexion) of the big toe, often with extension and abduction (“fanning”) of the other toes. This abnormal response is termed the extensor plantar response (Babinski reflex). [1]
The Babinski reflex was described by the neurologist Joseph Babinski in 1899. His main aim was to find objective signs to distinguish hysterical from organic paralysis. Since that time, it has been incorporated into the standard neurological examination. The Babinski reflex is easy to elicit without sophisticated equipment. Since it is a reflex, it does not require active patient participation and therefore can be performed in patients who are otherwise unable to cooperate with the neurological exam. [2]. However, few realize that it was Remak in 1893, who first reported the observation of an extensor plantar response in a patient suffering from transverse myelitis. [3]
Stroking the sole is easy enough; the importance of the method of stimulation has been grossly overrated. But it is not so simple to determine whether the resulting toe movements are normal or abnormal, even for neurologists. Some background information is essential. In some patients, a Babinski sign is an early and sometimes the only clue to an upper motor neuron lesion. [4]
Our aim of the article is to review the significance of this most commonly performed clinical test in medical/neurological practice. In the era where we are now more and more rely on modern investigations.
The Babinski reflex tests the integrity of the corticospinal tract. Fibers from the corticospinal tract synapse with the alpha motor neuron in the spinal cord and help direct motor function. The corticospinal tract is considered the upper motor neuron and the alpha motor neuron is considered the lower motor neuron. Sixty percent of the corticospinal tract fibers originate from the primary motor cortex, premotor areas, and supplementary motor areas. The remainder originates from primary sensory areas, the parietal cortex, and the operculum. Damage anywhere along the corticospinal tract can result in the presence of a Babinski sign. Stimulation of the lateral plantar aspect of the foot (S1 dermatome) normally leads to plantar flexion of the toes (due to stimulation of the S1 myotome). Nociceptive input travels up the tibial and sciatic nerve to the S1 region of the spine and synapse with anterior horn cells. The motor response which leads to the plantar flexion is mediated through the S1 root and tibial nerve. The descending fibers of the corticospinal tract normally keep the ascending sensory stimulation from spreading to other nerve roots. When there is damage to the corticospinal tract, nociceptive input spreads beyond S1 anterior horn cells. This leads to the L5/L4 anterior horn cells firing, which results in the contraction of toe extensors (extensor hallucis longus, extensor digitorum longus) via the deep peroneal nerve. An intact corticospinal tract prevents such spread.
The Babinski reflex should be elicited by a dull, blunt instrument that does not cause pain or injury. Sharp objects should be avoided. The dull point of a reflex hammer, a tongue depressor, or the edge of a key is often utilized.
The patient should be relaxed and comfortable. It is best to advise the patient that the sensation may be slightly uncomfortable. Patients may experience both a mildly unpleasant sensation as well as a tickling sensation. In my experience of clinical practice, it’s always wise to explain what the patient is going to feel. Because some time while performing the test patient gets feared and it led to further neurological examination difficult out of apprehension. Most clinicians agree that the site and intensity of stimulation are most important factors in eliciting the response correctly. To test for planter reflex, the instrument is run up the lateral plantar side of the foot from the heel to the toes and across the metatarsal pads to the base of the big toe. Care should be taken to avoid touching the toes. Many variations of the Babinski sign (extensor planter reflex) have been described. Each of them designed to elicit dorsiflexion of the big toe. The mechanism by which these alternatives elicit this response is likely similar to the Babinski response. These variations are useful in patients who have a significant withdrawal response to the conventional testing for the Babinski reflex. [2]
Clinical Significance of abnormal planter reflex is indicative of dysfunction of the corticospinal tract. Oftentimes, the presence of the reflex is the first indication of spinal cord injury after acute trauma. Care must be exercised in interpreting the results because many patients have significant withdrawal response to plantar stimulation. When this occurs, one of the variations on eliciting a Babinski sign can be utilized. In comatose patients, one may witness a triple flexion response. Care must be made to distinguish this from a withdrawal response. The triple flexion response is very stereotyped whereas the withdrawal response can vary with each stimulation. Healthcare workers should be aware of other methods of elicitation of the Babinski reflex, especially in patients with an absent toe or infection [2]
The normal response is plantar flexion of the great toe, which is considered an absent (negative) Babinski sign. Dorsiflexion of the great toe (Babinski sign present) suggests an upper motor neuron lesion and also is referred to as a positive Babinski sign. Dorsiflexion of the big toe also may be associated with fanning out of the other toes, as detailed in Babinski’s original description, but most neurologists consider this an unnecessary accompaniment of an abnormal response. [5]
The Babinski sign is seen when toe extension occurs due to stimulation of the “wrong” receptive field i.e., the sole. Therefore, application of a noxious stimulus at the sole produces toe extension in place of normal flexion. The underlying mechanism is thought to be Extensor Hallucis Longus recruitment, and consequent overpowering of toe flexors. It is noteworthy that movements of other joints are unaffected. [3]
The plantar reflex is a nociceptive segmental spinal reflex that serves the purpose of protecting the sole of the foot. The clinical significance lies in the fact that the abnormal response reliably indicates metabolic or structural abnormality in the corticospinal system upstream from the segmental reflex. Thus, the extensor reflex has been observed in structural lesions such as hemorrhage, brain and spinal cord tumors, and multiple sclerosis, and in abnormal metabolic states such as hypoglycemia, hypoxia, and anesthesia. The receptive field for the extensor plantar response can be quite extensive. On occasion the extensor reflex has been elicited by stimulating as high as the face. Even in the same individual there is often shrinkage in the receptive field as time passes after the occurrence of the lesion. The reflex response is on occasion equivocal. [1] Professor William Landau’s statement: “Plantar reflex patterns are not restricted to only two up-or-downs, chocolate-or-vanilla flavors”. [6] On occasion, the reflex may be unequivocally flexor on one side and the toe remains neutral without movement on the other side. Under these circumstances the question is whether there is evidence of corticospinal tract dysfunction, and not whether the response is flexor or extensor. This question can often be answered by looking for other evidence of corticospinal dysfunction, such as repeating deep tendon reflexes. [1]
- Why the toe goes up in abnormal planter response?
If one uses a fingernail to scratch the sole of a baby, not too gently (to avoid a grasp reflex), the result is flexion of the hip and knee, and dorsiflexion of the foot and toes, especially the great toe. This combined response is the so-called flexion synergy. Anatomists have attached the erroneous term ‘extensors’ to the muscles that move the toes up. As the baby grows older, the pyramidal system matures and increases its influence on the spinal cord, especially on the motor neurons of distal extremity muscles. For the flexion reflex of the leg these results in two changes. The first is that the synergy as a whole becomes less brisk, at least in most people. The second is that after the first year of life the toes no longer take part in the flexion synergy. After stimulation of the sole the toes move down, not up. If the pyramidal tract becomes damaged by disease, either structural or functional, the plantar reflex can revert to the ‘infantile’ type: the toe ‘extensors’ are again recruited into the flexion synergy of the leg. This is the sign of Babinski (Babinski 1896). [4] Not every up going toe is Babinski sign.
2. when is an up going toe a Babinski sign?
There are three requirements need to be met: [4]
(a)The tendon of the extensor hallucis longus muscle must be active.
(b) The upward movement of the great toe should coincide with contraction of other flexor muscles in the leg.
(c) It should be possible to elicit the phenomenon more than once. A great toe that keeps pointing up for some time after the stimulus indicates (more or less) voluntary withdrawal.
3. what is a complete response?
A complete response is constituted by contraction of Extensor Hallucis Longus, extensor digitorum longus, tibialis anterior, the tensor fascia lata and the hamstrings. The most important and definitive response is dorsiflexion of the great toe. The movement of the great toe also the first among all the movements [3]
4. Is there any normal physiological variation to reflex?
In infants with at corticospinal tract which is not fully myelinated the presence of a Babinski sign in the absence of other neurological deficits is considered normal up to 24 months of age. Babinski’s may be present when a patient is asleep. [2]
5. what are variants of the sign?
True: It has complete components of the fully developed extensor plantar reflex.
Minimal: Tensor fascia lata and hamstrings contract.
Pseudo: Seen in sensitive individuals. Constituted by plantar hyperaesthesia, and choreo-athetosis. It may be as a result of hyperkinesis.
Exaggerated: It is dependent upon which group of muscles has the dominant tone. It may be either ‘extensor spasm’ or ‘flexor spasm’. The former is seen is corticospinal pathology with normal posterior column, while the latter shows up in diseases like subacute combined degeneration, multiple sclerosis and spinal cord pathology.
Crossed extensor: Also called bilateral Babinski sign, it may be elicited in patients with bilateral cerebral and spinal cord pathology.
Tonic: In frontal lobe and extrapyramidal pathology, a slow and prolonged toe extension may be seen.
Spontaneous: In patients with extensive pyramidal tract pathology, passive hip or knee flexion may elicit a positive Babinski sign.
Inversion: In case of severance or paralysis of toe short flexors, an extensor response can be elicited
6. What the sensitivity of the planter response?
The utility of the plantar reflex in modern neurology is controversial. (Rui Araujo et al) studied the Babinski, Chaddock, and Oppenheim reflexes in terms of intra-observer, interobserver, and intertest agreement; sensitivity; positive predictive value (PPV); and observer bias. Sixty-two patients and 1,984 reflexes were analyzed. Intra-observer and interobserver agreement were weak. There was no evidence of observer bias. Sensitivity was 59.7% for the Babinski, 55.3% for the Chaddock, and 30.0% for the Oppenheim. PPV was 70.3% for the Babinski, 66.5% for the Chaddock, and 61.3% for the Oppenheim. [6]
7. Significance of equivocal (mute planter) response?
As a rule of thumb, a pathological plantar response (about which there is no disagreement) always indicates a disturbance of the pyramidal system, either structural damage or temporary disturbance due to epilepsy or intoxication. No convincing exceptions to this rule are known; in other words, the specificity of the sign is 100%. Conversely, in patients with lesions of the pyramidal tract about 10% will show a normal or at least mute plantar response (sensitivity of 90%) (Van Gijn 1978): one possible reason (not the only one) is a weak flexion synergy of the leg, which makes it impossible for the Babinski sign to emerge. [4]
8. what is a “Delayed plantar reflex”?
Delayed plantar reflex (DPR) is a pathologic flexor variant which requires unusually strong stimulation of the sole of the foot and is characterized by a prolonged interval between the stimulus and the response, slow and protracted plantar flexion of the great toe and/or other toes and slow return to the neutral position.
9. What is “triple flexor response”?
In this case, one observes dorsiflexion of the big toe, the fanning of the other toes, dorsiflexion of the foot, as well as knee flexion. The triple flexion response represents profound dysfunction of the corticospinal tract, with a spread of the reflex to the L3 and L2 myotomes. [2]
10. How to elicit the Babinski reflex in a patient with amputated leg?
Stroke on the stump of the imputed leg and watch for tensor fascia lata contraction: internal rotation of hip could be helpful, it’s regarded as Brissauds reflex, and the significance is the same.
11. What are the alternative methods / ‘Babinski like responses? [3]
Several dozen surrogate responses (with numerous eponyms) have been described over the years, most utilizing alternative sites and types of stimulation, but all have the same significance as the Babinski response. [8]
Chaddock’s Sign: Stroking the skin around the lateral malleolus in a circle.
Oppenheim’s Sign: Anterior surface of tibia is compressed by thumb and index finger.
Gonda’s Sign: Forceful stretching and snapping of the 2nd or 4th toe downwards.
Gordon’s Sign: Application of deep pressure to the calf muscle.
Schaeffer’s Sign: Application of deep pressure on the Achilles tendon.
Stransky Sign: Abduction and snapping of 5th toe.
Mendal Bechtrew Sign: Tapping of dorsum of foot over the cuboid bone.
Rossolimo’s Sign: Tapping the ball of the foot or flicking and snapping the distal phalanges of the toes into extension.
Moniz Sign: Ankle is forcibly and passively plantar flexed.
Bing’s Sign: Pricking of the dorsum of foot or the 1st toe with a pin.
Strumpell Sign: Deep pressure application on the anterior tibia.
Cornell Sign: Stroking the dorsum of foot along the extensor tendon of the 1st toe.
Brissaud’s reflex: In patients with a missing great toe or complete paralysis of toe extension, the contraction of tensor fascia lata can be observed.
Throckmorton: Hitting the metatarsophalangeal joint of the big toe.
12 are there any contraindications?
The only contraindication to performing the Babinski reflex is a lesion (such as an infection) in the affected area of the foot that precludes the effective performance of the reflex. In such situations, one of the alternative methods of eliciting the response may be done.
13. What to do, if unable to get a planter response?
In a suspected neurological problem if no abnormal response has been obtained, take a tongue blade and break it in half longitudinally and use the sharp point. The reason for the graded stimuli is twofold: (1) Light touch, as with a finger, frequently obtains the reflex without causing a withdrawal response that on occasion makes interpretation of the response difficult; (2) one cannot conclude the response is normal until a noxious stimulus is indeed used, since the reflex is a cutaneous nociceptive reflex. The first line to be stroked begins a few centimeters distal to the heel and is situated at the junction of the dorsal and plantar surfaces of the foot. The line extends to a point just behind the toes and then turns medially across the transverse arch of the foot. Stroke slowly, taking 5 or 6 seconds to complete the motion. Do not dig into the sole, but stroke. Successive lines are stroked, each about 1 cm medial to the preceding stroke, until the examiner is stroking the midline of the foot. The occurrence of the extensor response on any of these lines is abnormal, even if the response is flexor on another line of stroking. This variation relates to variability in the receptive field of the reflex, undoubtedly due to the extent of corticospinal involvement as well as individual differences. The reflex is normal if the abnormal response is not obtained from any of the stroke lines using all of the stimuli described. A good habit is to describe whatever response is obtained in addition to noting whether in your opinion the response is normal or abnormal. [1]
There is petite doubt that the fascinating Babinski sign holds great clinical implication in practice. Extensor planter response points towards withdrawal of supraspinal control over the flexor reflexes. The plantar reflex is often discussed alongside deep tendon reflexes, but it is a cutaneous reflex. If the great toe consistently goes up (dorsiflexes, Babinski’s sign) then a lesion of the upper motor neuron is present (flexion withdrawal due to ticklishness or hypersensitivity can be confounding factors). There is some evidence that neurologists’ interpretation of the plantar reflex is influenced by their presuppositions based on the clinical history. [7]
References:
[1] Walker HK, Hall WD, Hurst JW. The Planter Reflex. In: Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd Ed. Boston
Butterworths; 1990.
[2] Aninda B. Acharya, Radia T. Jamil, Jeffrey J. Dewey. Babinski Reflex. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2022. PMID: 30085551
[3] Paurush Ambesh, Vimal Kumar Paliwal, Vijay Shetty, Stephan Kamholz. Review Article the Babinski Sign: A comprehensive review; J Neurol Sci. 2017 Jan 15; 372: 477-481.
[4] Jan van Gijn. Neurological sign: The Babinski sign; Practical Neurology. 2002:42-44.
[5] Kalarickal J Oommen. Medscape-Neurological History and Physical Examination. 2021. www.emedicine.medscape.com
[6] Rui Araújo, MD, João Firmino-Machado, MD, Pedro Correia, et al. The plantar reflex A study of observer agreement, sensitivity, and observer bias: Neurol Clin Pract. 2015; 5(4): 309–316. PMID: 29443235.
[7] A J Lees, Brian Hurwitz. Testing the reflexes: Practice Essentials; The BMJ 2019; 366:14830
[8] Adams & victors Principles of Neurology. Approach to the patient with neurologic Disease, 11th Ed. London: Mc Graw Hill Education; 2019.