Heart Failure With Preserved Ejection Fraction: Diagnostic And Treatment Management Strategies
* Sam Gamlin
*Post-graduate Resident, Lady Hardinge Medical College
https://meditropics.com/heart-failure-with-preserved-ejection-fraction/
INTRODUCTION
Heart failure is a major cause of mortality and morbidity with a lifetime risk at age 40 years of approximately 20%.1 Heart failure with preserved ejection fraction (HFpEF) now accounts for more than 50% cases of Heart failure2 with outcome comparable to Heart failure with reduced ejection fraction (HFrEF).3 They are often underlooked and results in delay in management. Fortunately recent advances regarding pathophysiology of HFpEF, improved methods of diagnosis and prognostic predictions now can yield effective treatment strategies.
But still challenges remain in terms in managing HFpEF. There is no definite single test that establishes its diagnosis, so it becomes absolutely necessary to consider potential mimics both cardiac and non cardiac, that may present with signs of congestion and/or symptoms of dyspnea, exercise intolerance or congestion with preserved ejection fraction. These mimics have distinct pathophysiological mechanisms and require disease directed management.
Clinicians must also consider the role comorbidities that contribute to symptoms and prognosis.
Challenges of HFpEF are even more difficult in women as they have more preserved left ventricular global longitudinal strain and higher ejection fractions compared to men4 , thereby making them less likely to develop a reduced ejection fractions. Women have a lifetime risk for Heart failure of approximately 20% by age 40 years, increasing to nearly 30% by age 55 years.5
2 DIAGNOSIS OF HFpEF
Framingham Heart Failure Diagnostic Criteria defines Heart failure as presence of 2 or more major criteria or 1 major criteria plus 2 minor criteria. Major criteria include orthopnea, jugular venous dissension, hepatojugular reflux, rales, S3 gallop rhythm, acute pulmonary edema, and cardiomegaly. Minor criteria include dyspnea on exertion, nocturnal cough, and ankle edema, tachycardia with heart rate over 120 beats per minute, hepatomegaly and pleural effusion.
The Universal Definition of Heart Failure requires symptoms and/or signs of Heart failure, as outlined earlier and at least 1 of the following: 1) Elevated Natriuretic peptides 2) Objective evidence of cardiogenic pulmonary or systemic congestion.
While the above definitions help in guiding clinicians, establishing a diagnosis of HFpEF is more difficult as echocardiogram may not demonstrate obvious structural or functional cardiac abnormalities and the natriuretic peptide levels may be normal, especially in obese individuals.
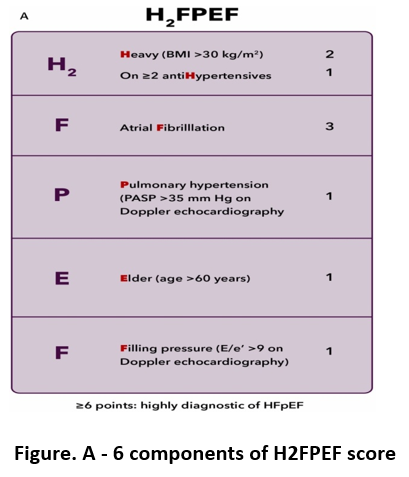
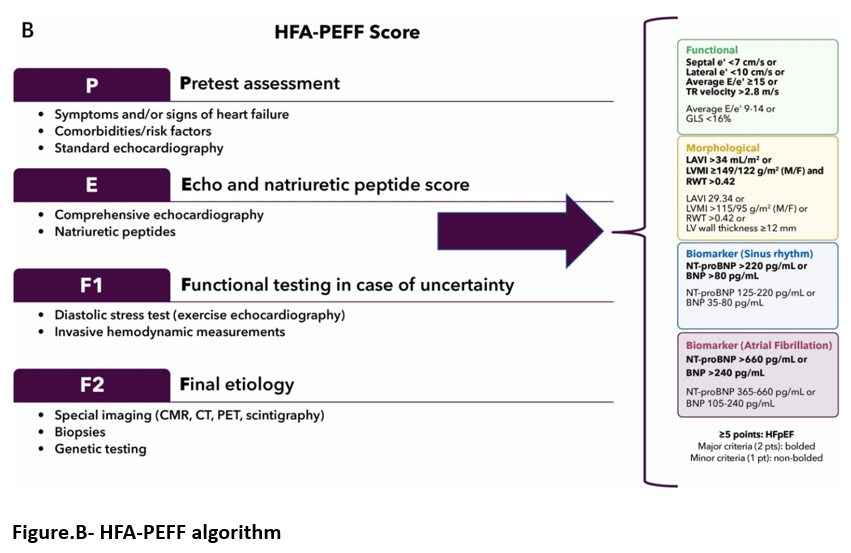
Given the lack of definitive testing modalities the use of clinical scoring systems and algorithms H2FPEF and HFA-PEFF aid in the diagnostic evaluation of suspected HFpEF. 6 The H2FPEF score uses a gold standard reference of invasive exercise hemodynamic measurements and is a more practical system for clinicians.
The 6 components of H2FPEF score consist of: Heavy body (BMI >BMI kg/m2) , Hypertension (on 2 or more antihypertensive medication), atrial fibrillation, pulmonary hypertension (estimated pulmonary artery systolic pressure >35 mm Hg on doppler echocardiography), elder(age >60 years), Filling pressures ( E/e’>9 on dappled echocardiography) ( Figure A).A score of 6 or higher is highly suggestive of HFpEF.
The HFA-PEFF algorithm includes 4 steps: Step 1 is the pretest assessment is to identify individuals who may have HF based on clinical assessment and standard diagnostic tests like natriuretic peptides, electrocardiogram, and echocardiograms. Step 2 is echocardiographic and natriuretic peptides score, with points assigned based on there findings. Step 3 is functional testing in case of uncertainty including a diastolic stress test with exercise stress echocardiography followed by invasive hemodynamic monitoring. Step 4 is final etiology, including testing to rule out other cardiac causes of dyspnea and /or edema such as pericardial disease, valvular disease, infiltrative/restrictive cardiomyopathy.( Figure B)
MANAGEMENT OF HFpEF
Managementfocuses primarily on : 1) Risk stratification and manage net of comorbidities including hypertension, Diabetes, obesity etc ; 2) Nonpharmacological management like role of exercise and weight loss, implantable pulmonary artery monitors ; 3) Symptom management and disease modifying therapy.
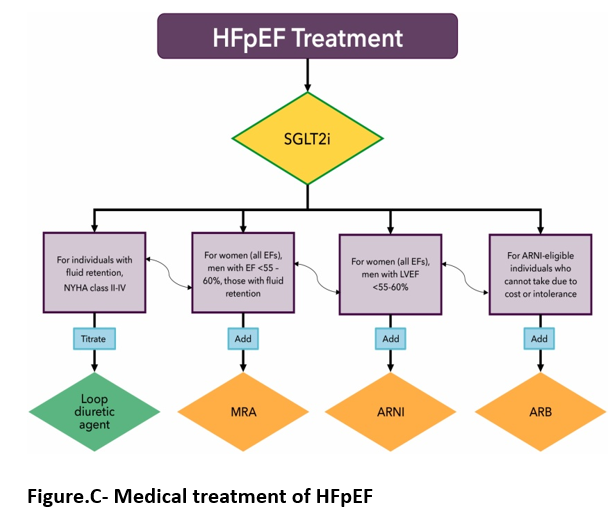
Medical therapy for HFpEF (Figure C)
Recent trialshave shown the benefit of medications in individuals of HFpEF and its initiation is key in improving symptoms and reducing mortality and morbidity. Drugs used are loop diuretics agents, SGLT2 inhibitors, mineralocorticoid antagonists (MRA), angiotensin receptor -nephrilysin inhibitors (ARNIs), and angiotensin receptor blockers (ARBS).
Beta blockers may be used in individuals with HFpEF who have specific indications like prior myocardial infarction, angina, or atrial fibrillation.
All individuals should be treated with SGLT2i barring contraindications, with goals of decreasing morbidity and mortality. In those with LVEF <50% to 60% use of MRA, ARNI, or ARB may be considered. ARNIs and MRAs should be titrated to maximum tolerated doses based on symptoms , blood pressure, potassium, and creatinine.
Special note is made for women with HFpEF where SGLT2i is an expected component of treatment barring contraindications, use of Sacubitril/valsartan as well as spironolactone should be considered across the entire LVEF spectrum. Reason why women respond more favorably to therapies at higher ejection fraction may be because they tend to have smaller LV chamber size and thus are prone to demonstrate higher LVEF when compared to men. Therefore LVEF of 50% to 55% in a women may be abnormally low compared to men.
Other Non-pharmacological Management
This includes strategies to target contributing comorbidites, such as Hypertension, obesity and also exercise, weight loss and to guide and titrate pharmacological therapies with pulmonary artery sensor monitoring. In particular, physical inactivity and obesity are linked with poorer outcome in HFpEF. Regular self-monitoring of food intake, weight and physical activity, preferably aerobic (eg brisk walking) for >150 minutes/week (equal to >30 minutes/day on most days) is recommended for initial weight loss.
Regarding pulmonary artery pressure monitoring via implantable device, in 2022 AHA/ACC/HFSA HF guideline has given a class 2b recommendation.
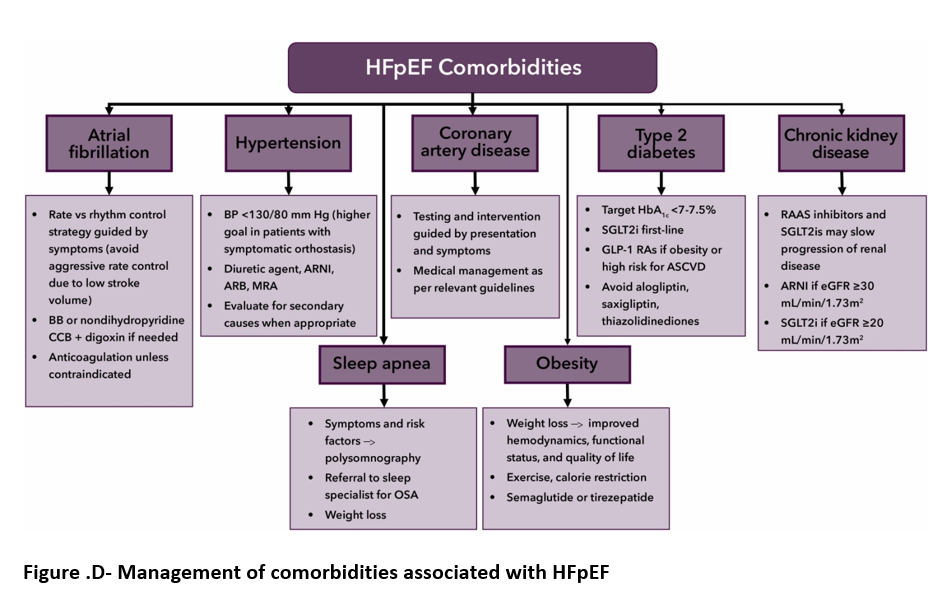
A summary table of management of comorbidities associated with HFpEF is given below (Figure D)
Conclusion – Decisions taking can be complex and require early and accurate detection and careful monitoring to provide the most effective recommendations and prevent morbidity and mortality in the long term.
Abbreviation
ACC = American College of Cardiology
ACE = Angiotensin converting enzyme
AF = Atrial Fibrillation
ARB = Angiotensin receptor blocker
ARNI = Angiotensin receptor-neprilysin inhibitor
EF = Ejection fraction
HF = Heart failure
HFpEF = Heart failure with preserved ejection fraction
NT-proBNP = N-terminal pro-B-type natriuretic peptide
SGLT2i = sodium glucose cotransporter-2 inhibitor
T2DM = Type 2 diabetes mellitus
References
- Januzzi J.L., Ahmad T., Binder L.G., et al.”2019 methodology for creating expert consensus decision pathways: a report of the American College of Cardiology”. J Am Coll Cardiol. 2019;74:1138-1150.
- Virani S.S., Alonso A., Benjamin E.J., et al.”Heart disease and stroke statistics-2020 update: a report from the American Heart Association”. Circulation. 2020;141:e139-e596.
- Shah K.S., Xu H., Matsouaka R.A., et al.”Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes”. J Am Coll Cardiol. 2017;70:2476-2486.
- Chung A.K., Das S.R., Leonard D., et al.”Women have higher left ventricular ejection fractions than men independent of differences in left ventricular volume: the Dallas Heart Study”. Circulation. 2006;113:1597-1604.
5.Lloyd-Jones D.M., Larson M.G., Leip E.P., et al. “Lifetime risk for developing congestive heart failure: the Framingham Heart Study”. Circulation . 2002;106:3068-3072.
- Reddy Y.N.V., Carter R.E., Obokata M., et al.”A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction”. Circulation. 2018;138:861-870.