Adverse effects of blood transfusion
https://meditropics.com/652-2/
Deepika Bhardwaj
Post graduate resident, Department of Medicine, LHMC
Adverse effects of blood transfusion are most commonly seen in patients requiring repeated and large numbers of transfusions. These can be divided into immediate and delayed.
Immediate transfusion reactions can be further divided as:
- A) Immunological transfusion reactions
- Immediate haemolytic transfusion reactions
- Febrile non-haemolytic transfusion reactions
- Transfusion-related acute lung injury
- Allergic reactions
- B) Non-immunological reactions
- Transfusion-associated circulatory overload
- Hypothermia
- Hyperkalemia
- Hypocalcemia
Immune-mediated transfusion reactions
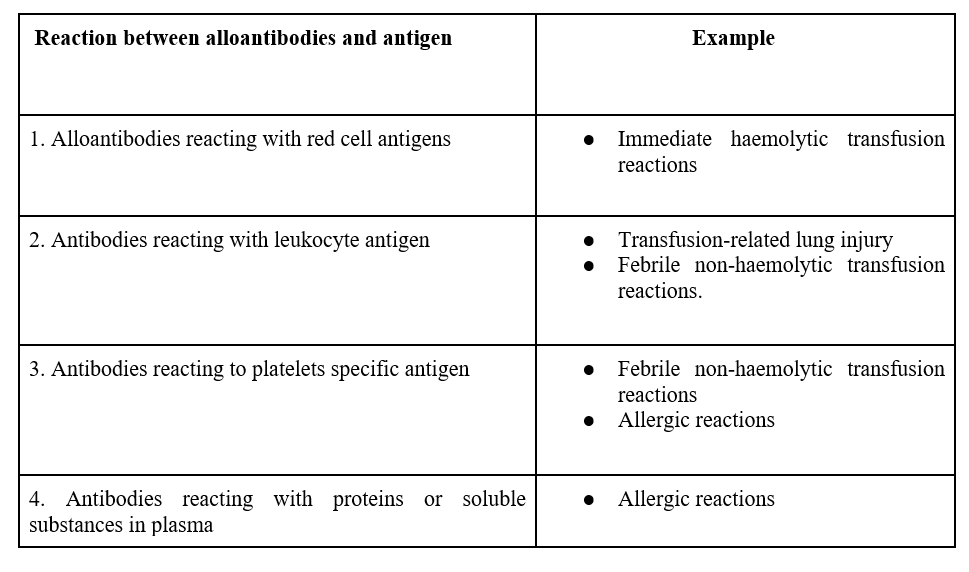
In an immune-mediated transfusion reaction, alloantibodies react with antigens present on different blood components, which can be summarized below
Hemolytic transfusion reactions
Immediate (intravascular ) haemolytic transfusion reactions
These reactions are most commonly associated with ABO incompatibility and Kell (K). Anti-A and anti-B are IgM antibodies that bind to the complement system leading to devastating intravascular hemolysis.
It occurs soon after the transfusion begins.
Symptoms and signs-
The most common symptom is fever with or without chills. Other symptoms can be anxiety, chest and back pain, flushing, and dyspnea. On examination, tachycardia and hypotension can be present.
Management – Stop ongoing blood transfusion immediately.
Recheck of patient’s identity with discontinued blood and report to the blood bank without delay. Send post-transfusion blood samples and discontinued blood units to the blood bank. Normal saline should be infused to maintain blood pressure and urine output and in case of a hemostatic defect, transfuse cryoprecipitate, platelets, and plasma.
Complications – this transfusion reaction can lead to acute renal failure, shock, and disseminated intravascular coagulation.
Febrile nonhemolytic transfusion reactions
These reactions are the results of Alloimmunization to antigen on leukocytes and platelets.
Symptoms – a) chills followed by a fever of more than and equal to 1°C, b) headache and c) nausea and vomiting.
Management – Discontinue ongoing blood transfusion immediately. Bacterial contamination and hemolytic reaction should be ruled out. Antipyretics like acetaminophen or hydrocortisone can be given. Meperidine can be given to decrease severe shaking chills. Antihistamines can be used if the patient has allergic symptoms like hives.
Prevention – febrile nonhemolytic transfusion reactions can be prevented by using leukoreduced red cells.
Transfusion-related acute lung injury (TRALI)
Transfusion-related Acute lung injury is an acute lung injury within 6 hours of transfusion, characterized by acute onset hypoxemia with PaO2/FiO2 ≤ 300 with bilateral lung infiltrates and no evidence of circulatory overload.
Two event hypothesis – according to this TRALI is comprised of two events,
The first event is patient-related, like underlying sepsis/hematological disease/post-surgical status and the second event is related to the transfusion of potential granulocytes primers like cytokines/lipids and alloantibodies.
Symptoms and signs – Sudden development of shortness of breath, fever, severe hypoxemia (O2 saturation <90% in room air), and low blood pressure. In some cases, patients can also have high blood pressure.
Management– Management consists of supportive measures for pulmonary edema and hypoxemia and hypotension. Sometimes the patient may require mechanical ventilatory support.
Prevention – TRALI can be prevented by screening donors for granulocyte-specific and HLA antibodies that react to recipient leukocytes and avoiding further transfusion from implicated donors.
Allergic reactions
Allergic reactions occur because of IgE antibodies against proteins and other soluble substances in donor plasma which leads to histamine release.
Symptoms and Signs – Allergic reactions can range from minor urticarial skin lesions and skin rashes to bronchospasms, angioedema, and anaphylactic shock.
Minor urticarial reactions are the only transfusion reactions that do not necessitate immediate discontinuation of transfusion.
Treatment – Patients can be Premeditated with H1 blocking agents (diphenhydramine 50 mg orally/IM). Allergic reactions can be reduced by decreased plasma content of transfused blood products.
Management of anaphylactic reactions is very crucial as this can be fatal. Management includes early detection and prompt treatment. Symptoms of anaphylactic reactions can be difficulty breathing, coughing, nausea, vomiting, hypotension, bronchospasm, respiratory arrest, and shock. Treatment includes immediately stopping blood transfusion, maintaining vascular access, and administering epinephrine 0.5 to 1ml of 1:1000 dilution subcutaneously. Glucocorticoids can be given in severe cases.
Prevention – Individuals with severe IgA deficiency should receive IgA-deficient plasma and washed cellular blood components
Transfusion-associated circulatory overload (TACO)
Transfusion-associated circulatory overload is characterized by increased central venous pressure, left heart failure, positive fluid balance, pulmonary edema and raised BNP levels within 6 hours of transfusion.
Symptoms and signs – Patients can have complaints of shortness of breath along with signs of excess fluid within the circulatory system, i.e., leg swelling, high blood pressure, Tachycardia, raised JVP, inspiratory crackles and an S3 murmur.
Management – management of Transfusion-associated circulatory overload revolves around decreasing systemic congestion, including stopping ongoing blood transfusion and administering diuretics and oxygen.
Prevention– The cornerstone of preventing transfusion-associated circulatory overload is to Identify patients at risk. This includes old age, cardiac dysfunction, renal dysfunction, and fluid overload condition. These patients should receive small-volume blood transfusion with careful monitoring.
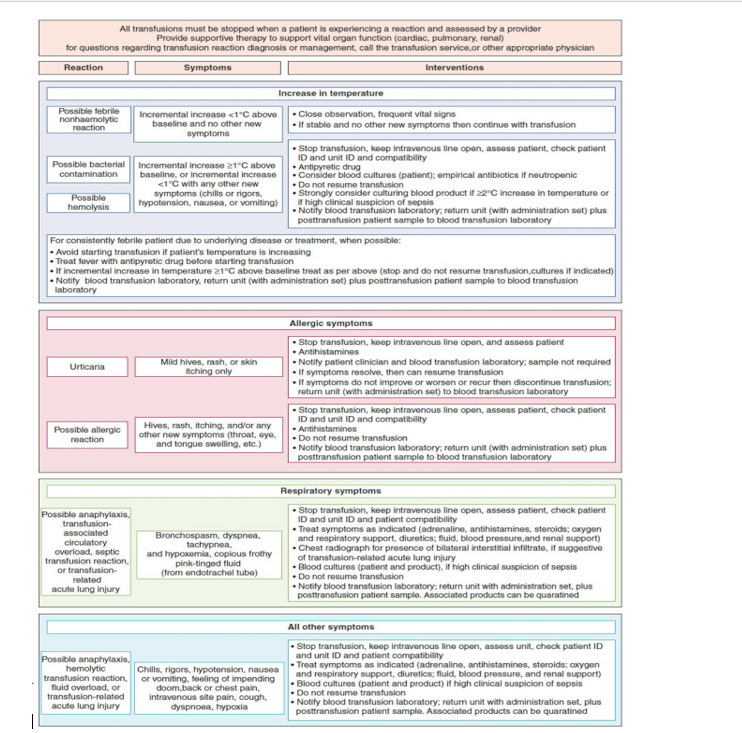
Fig. 1. Transfusion reaction decision tree. Algorithm to guide assessment and actions to take when a transfusion reaction is initially identified. Actions should go from left to right.
Metabolic effects and hypothermia
Metabolic effects mainly include Hyperkalemia and Hypocalcemia.
Hyperkalemia
Hyperkalemia is defined as levels above 5.5 mmol/L.
Risk factors – Risk factors for Hyperkalemia include longer storage, irradiation of blood components, and rapid transfusion of large volumes of blood.
Symptoms and signs – symptoms and signs of hyperkalemia vary with the degree of hyperkalemia, i.e., mild, moderate, or severe. These can range from nonspecific symptoms like tiredness, numbness and weakness to life-threatening arrhythmia and sudden cardiac arrest. An electrocardiograph should be obtained to identify changes in the myocardium.
Treatment – Treatment of Hyperkalemia includes stabilizing the cardiac membrane with the injection of calcium gluconate and instituting potassium lowering therapy which includes diuretics, insulin and dextrose and beta agonist.
Hypocalcaemia
Hypocalcemia is defined as levels less than 2.1 mmol/L.
Hypocalcemia occurs due to a significant amount of citrate in the blood.
Symptoms and signs – Patients can have numbness and carpopedal spasm, paresthesia (oral, perioral, acral), convulsions and cardiac dysfunction (arrhythmias). Patients can show the Trousseau sign and the Chvostek sign.
Treatment – Hypocalcemia should be treated with calcium infusion.
Hypothermia
Hypothermia is defined as a body core temperature below 35.0 °C (95.0 °F).
Hypothermia occurs due to the transfusion of a large volume of cold blood. It is commonly seen in neonates and the elderly.
Hypothermia interferes with platelet and clotting function.
Symptoms and signs- Affected individuals with Mild hypothermia generally have shivering, high blood pressure, tachycardia, tachypnea and hyperglycemia. Moderate hypothermia leads to altered mentation, and decreased reflexes, while severe hypothermia can further lead to bradycardia, hypotension, and depressed respiration function.
Treatment – Treatment of hypothermia includes an infusion of warm saline and blood and using warm devices.
References:
1) Wintrobe’s clinical hematology 14th edition.
2) Harrison’ principle of internal medicine 21st edition.