Storage of Blood Components and its Significance
https://meditropics.com/668-2/
Rohan Sharma
Post Graduate Resident, Department of Medicine, LHMC
- Introduction
The primary objective of preservation, storage and transportation of blood and blood components is to preserve the viability and function of each relevant constituent, prevent any physical changes of the blood constituent during storage and minimize bacterial growth.
Various anticoagulant-preservative mixtures have been formulated with the ultimate goal of preventing clotting and to provide proper nutrition for cell metabolism during storage. This ensure that blood and blood components are kept therapeutically viable for a stipulated time.
- Anticoagulation and Preservation
Various anticoagulant-preservative solutions have been formulated for better red cell preservation, which are as follows
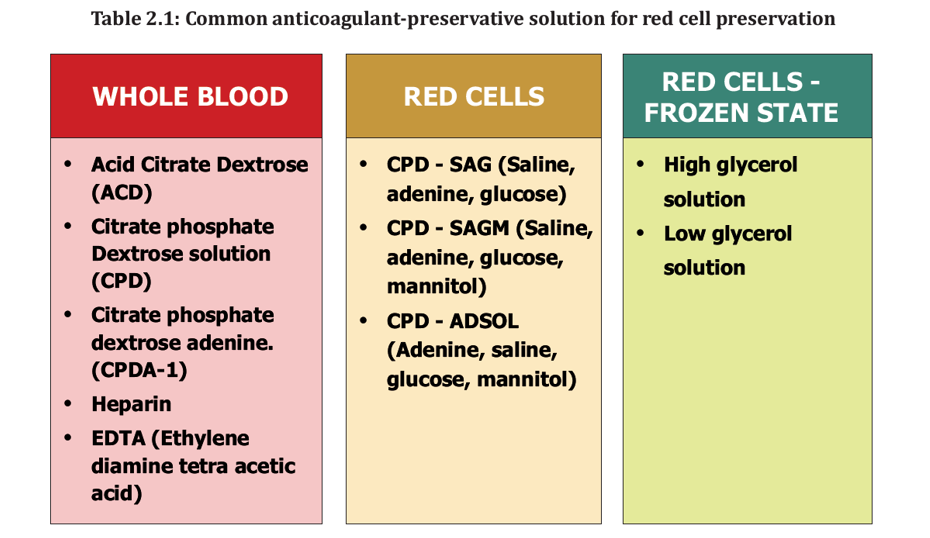
- Preservation of Whole blood
Citrate Based Anticoagulants. The important citrate-based anticoagulant – preservative solutions used are ACD, CPD, and CPDA (CPDA-1 and CPDA-2).
- Acid citrate dextrose (ACD):
The most widely used ACD solution has the following formula:
Trisodium citrate 22.0g
Citric acid (monohydrate) 8.0 g
Dextrose (monohydrate) 24.6 g
Distilled water to make up to 1 Litre
For each 100 ml of blood, 15 ml of the ACD solution (pH 5.0) is sufficient (e.g. for 450 ml, 67.5 ml of ACD solution is required).
ACD – Mechanism of Action
- Citrate (calcium Chelator) –
- Prevents coagulation
- Retards glycolysis
- Improves red cell viability
- Provides energy for ATP synthesis
- Decreases rate of hydrolysis of phosphorus
- Citric Acid
- Prevents glucose caramelization during autoclaving
- Provides optimal pH with citrate for red cells
Shelf life of whole blood / red cells in ACD = 21 days
(> 70% transfused cells viable after 24 hours)
- Citrate phosphate dextrose (CPD) :
CPD Solution
- Decreases acidosis
- Improves ATP synthesis
Shelf-life of whole blood in CPD = 28 days
- Citrate Phosphate Dextrose Adenine (CPDA):
Adenine
- Helps maintain high ATP levels
- Blood collected in CDPA
- safe
- well tolerated
- 2,3 DPG levels can be maintained for 12-14days
Shelf-life of whole blood in CPDA = 35 days
For both CPD and CPDA solutions, 14 ml (pH 5.6 to 5.8) of the solution is added for each 100 ml of blood.
- Preservation of Red cells – Optimal Additive Solution (OAS)
Different types of additive systems are now in use. These solutions contain saline, adenine and glucose and are added to the red cells after separating them from plasma. The advantages of using optimal additive solution (OAS) to red cells are as follows:
- Volume (ml) = Better storage condition for red cell preparation and lowering of
viscosity for ease of transfusion.
- Increased yield of plasma for plasma fractionation.
- Removal of unwanted buffy coat
- Additional 7-day storage time for red cell preparation
- Avoid unnecessary transfusion of plasma
Blood is collected into a multiple bag system including one plastic bag containing 100 ml of optimal additive solution.
After collection the whole blood is centrifuged and maximum amount of plasma along with the buffy coat is expressed into a transfer bag for further processing. Red cells are now suspended by running down the optimal additive solution (100 ml) to the main bag containing the red cells.
Currently available additive solutions are
- CPD-SAG (Citrate phosphate dextrose – saline, adenine, glucose) – In this besides CPD as the primary anticoagulant, a satellite bag contains the additive solution – 100 ml physiological
saline with adenine and glucose. CPD-SAG causes undesirable amount of haemolysis.
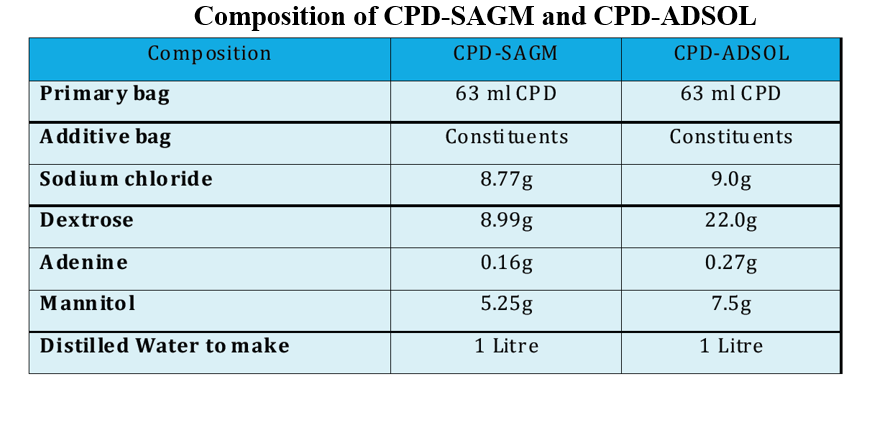
- CPD-SAGM– In this, the additive solution also has Mannitol to prevent lysis of red cells. The mean 24 hr. post transfusion survival is better with the additive.
- CPD-ADSOL– This additive solution is similar to CPD-SAGM but has greater quantities of glucose, adenine and Mannitol. It has better red cell preservation and 24 hr post-transfusion survival. The shelf life with this solution can be increased to 42-49days.

3) Preservation of Red Cells – Freezing (for Prolonged Storage)
Red cells can be stored for longer period in frozen state. Frozen red cells improve cell survival and increase shelf life to 5 years or more. It has been seen that freezing and subsequent thawing of red cells produces cellular dehydration and mechanical trauma due to intracellular ice formation which ultimately causes haemolysis.
A cryoprotective agent can prevent this freezing injury. The two agents commonly in clinical use are:
- Glycerol
- Dimethyl sulphoxide (DMSO)
Advantages and Disadvantages of Freezing of red cells
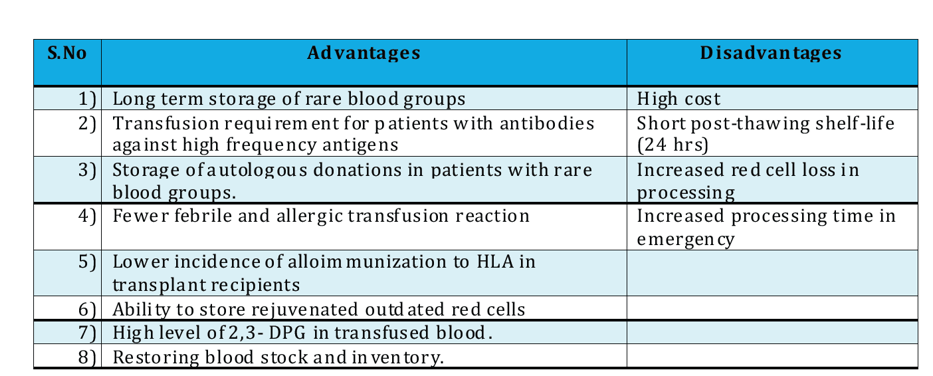
For freezing, red cells are used within 6 days of collection, however if a rejuvenating solution is used, the cells can be frozen even 2-3 days after expiry.
Two commonly used methods for freezing by glycerol employ:
- Low glycerol solution (20%)
- High glycerol solution (40%)
The rate of freezing and storage temperature determine the optimal glycerol concentration.
- Effects of Storage on blood components
- Effect of mixing red cell during storage
Red cells stored in SAGM or ADSOL show less spontaneous lysis and show fewer micro vesicles if the suspension is mixed, probably because of the dissipation of acid metabolites on mixing, which collect in the bottom layer of stored red cells.
- Physical and Biochemical Effects of Storage
The conditions of storage will invariably produce changes in the physical and chemical properties of blood and blood components and in turn effect red cell recovery.
Abnormalities resulting from storage of blood are collectively known as storage lesions
- Storage lesions
- Effect of collection on red cell recovery
The cells drawn at the start of donor bleeding are subjected to an acidic and hypotonic
anticoagulant solution which results in irreversible damage to some of the cells. These cells, in contrast to those drawn towards the end of phlebotomy, deteriorate more rapidly on storage.
- Effect on red cell function and survival
- Storage effect on red cell metabolism: The red cell is dependent on anaerobic glycolytic
pathway for the formation of ATP, which plays a central role in determining its viability and
maintaining its shape. During preservation the metabolic cycle must continue in vitro for
red cells to remain viable with adequate post transfusion survival and function.
- Effect on Oxygen release and 2, 3 Diphosphoglycerate (DPG): 2,3-DPG is known to profoundly lower the affinity of Hb for O at concentration found in red cells. Depletion of 2,3-DPG in stored blood temporarily adversely affects oxygen release by Hb.
- Effect on survival: In almost all cases, cells that survive 24 hrs will remain viable and
circulate for the remainder of their expected life span.
Maximum allowable storage time, referred to as shelf life is defined by requirement of 70%
recovery at 24 hrs i.e. at least 70% of the transfused red cells remain in the recipient’s
circulation 24 hrs after transfusion.
- Effect of anticoagulant-preservative
One of the most important factors influencing red cell recovery after blood storage is the
anticoagulant solution used.

- Effect on pH
There is a gradual fall in pH during storage due to accumulation of lactic acid.
- Effect of temperature
Optimum storage temperature for whole blood and red cells is between 2 ͦ -6 ͦ C with occasional elevation to 10 ͦ C (e.g. during transportation) being acceptable.
Delaying refrigeration increases the loss of 2,3-DPG over this period.
Platelets and granulocyte retain better function when stored at room temperature.
Labile coagulation factors in plasma are best maintained at temperature of -20ͦͦ ͦ C or lower.
Refrigeration and freezing additionally minimize proliferation of bacteria that might have
entered the unit during venepuncture.
- Effect on electrolytes & coagulation factors
- Electrolytes: The only important electrolyte change in stored blood is that of Potassium. During blood storage there is a slow but constant leakage of K+ from cells into the surrounding plasma. In severe kidney disease even small amount of K+ fluctuations can be dangerous and relatively fresh or washed red cells are indicated. Due to a higher K+ content of stored blood, blood < 5 days old is recommended for neonatal exchange and top-up transfusion.
- Coagulation factors: Labile coagulation factors, Factors V and VIII lose their activity by 50% within 48-72 hrs of storage.
- Effect on cellular elements
White cells lose their phagocytic and bactericidal property within 4-6 hrs of collection and
become non-functional after 24 hrs of storage. It is important to remember that they do not
lose their antigenic property and are capable of sensitizing the recipient to produce nonhemolytic febrile transfusion reactions.
Few lymphocytes may remain viable even after 3 weeks of storage.
Platelets lose their haemostatic function within 48 hrs in whole blood stored at 4 C.

- Rejuvenation of Stored Red Cells
Storage of RBCs causes reduction in the intracellular levels of 2,3-diphosphoglycerate (2,3-DPG) and adenosine triphosphate (ATP). Stored red cells even at the end of their allowable shelf-life can be rejuvenated with solutions containing pyruvate, inosine, phosphate and adenine. Incubation with the rejuvenating solution at 37 ͦC for 3-4 hours greatly improves viability and restores 2,3 DPG levels.
Method:
1) Add 50 ml of rejuvenating solution to the red cell concentrate.
2) Incubate at 37 ͦC for 1 hr prior to glycerolization and freezing.
Before transfusion, rejuvenated RBCs are to be washed to remove the rejuvenation solution. The
rejuvenated RBCs can also be frozen for long term storage. At the time of transfusion,
deglycerolization is performed, which accomplishes the removal of the rejuvenation solution and the glycerol.
RBCs preserved in CPD or CPDA-1 can be rejuvenated up to 3 days after the expiration date of the RBCs as long as the storage conditions are met. RBCs preserved in ADSOL maybe rejuvenated until 42days, but not after the expiration date. Rejuvenated CPD or CPDA-1 RBCs can be maintained in frozen storage for10 years; and ADSOL preserved RBCs can be stored frozen for only 3 years.
- Storage of Blood and Blood Components
After the processing of blood into blood components safe and adequate storage and transportation are of immense value to preserve the viability and therapeutic efficacy of the components during their shelf-life or till the time it is transfused to the recipient.
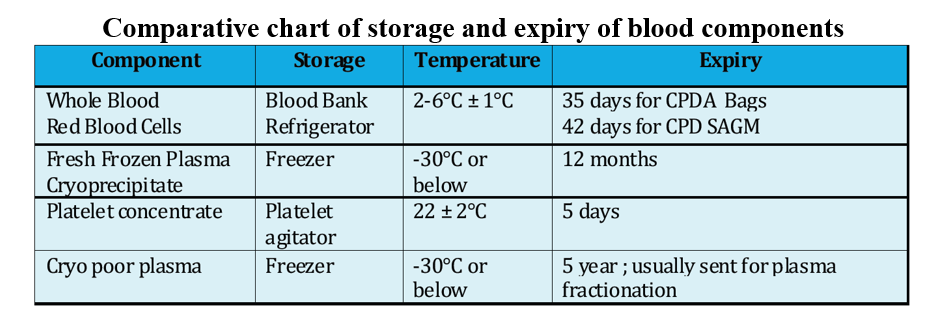
- Whole blood
Whole blood and red cell concentrate must always be stored between 2 ͦC and 6 ͦC. A fall in temperature less than 20 ͦC can cause freezing injury to the red cells leading to haemolysis. If homolysed blood is transfused to a patient; it can lead to fatal consequences.
Temperature more than 6 ͦ C can lead to overgrowth of bacteria, which may have entered the blood unit during collections or component preparation.
As red cells consume glucose for their continued metabolism, storing a blood unit at 2 ͦ- 6 ͦC will also decrease the rate of glycolysis. The shelf life of whole blood and red cell concentrate in commonly used anticoagulant, CPDA-1 is 35 days.
- Fresh frozen plasma (FFP)
frozen plasma is prepared by removing plasma from a unit of blood within 6 hours of collection and snaps freezing it to – 30 ͦ C.
The speed of freezing is very important for maintaining the coagulation factors. FFP must always be stored at – 20 ͦC or lower, otherwise the amount of clotting factors such as VIII and V will be greatly reduced.
FFP should preferably be stored in cardboard boxes (containing full information about the ABO blood group, donation unit number and screening test results,) to prevent fixing up with the adjacent bags while freezing, as it may lead to breakage of the bag. Packing should be in manner to leave tubing indent on frozen plasma.
Bag containing FFP meant for preparation of cryoprecipitate should be placed in between aluminium metal plates, to achieve a uniform thickness of plasma, which helps in rapid core snap freezing essential to maintain high yield of VIII in the cryoprecipitate.
- Platelets
Platelets are usually stored as concentrates. They are harvested from a single unit of blood either from PRP (platelet rich plasma) or from buffy coat and resuspended in 50 ml of autologous plasma.
Platelets should be stored at 22 ͦC in plasma under conditions in which the pH is maintained at values above 6.8. Shelf life of platelet concentrate is no more than 5 days in platelet storage bag. The functional integrity of platelets depends on many factors.
Storage temperature: Ideal temperature for platelet storage is 20 ͦto 24 ͦC. Temperatures below
20 ͦC during platelet preparation and storage cause a striking increase in the number of large
aggregates in the platelet-rich plasma.
pH: A fall of pH of platelet concentrate due to lactate production from platelet glycolysis leads to loss of viability. The rate of fall of pH is affected by:
- Number of platelets
- Volume of plasma in which stored
- Availability of O2
Plastics: Type of plastics used for storage of platelets is important. Availability of plastics with an increased permeability to Oxygen has made it possible to lengthen the period to which the platelets may successfully be stored. New second generation plastics such as polyolefin allow satisfactory storage up to 5 days. Platelet storage bag are marked with platelet or ‘5’ mark.
Agitation: Platelet concentrates must be gently and constantly agitated either on a flatbed agitator for better viability. Without agitation, there is a rapid fall in pH, due to collection of lactic acid metabolites.
Contamination with leucocytes: leucocyte contamination is associated with:
- Fall in pH.
- Loss of glycoprotein-lb (GP-Ib) from platelet surface leading to loss of platelet responsiveness to ristocetin and thrombin.
- Granulocytes
Granulocytes are stored generally in the same medium in which they are collected i.e. citrated donor plasma containing hydroxyl ethyl starch. Leucocytes tolerate storage poorly and lose their highly integrative function i.e. chemotaxis, within 24 hrs.
Storage is better at 20 ͦto 24 ͦC rather than 4 ͦC.
Granulocyte concentrate should be transfused as soon as possible and should not be stored for more than 1 day.
Bibliography
- Handbook on Component Preparation for BCSU: 2015. (n.d.). Retrieved November 24, 2022, from http://naco.gov.in/sites/default/files/FINAL%20BCSU_HANDBOOK%2014%2010%202015.pdf