Shivraj Meena(1), Bhawna Satija(2), Rashmi Rajput(3), Riya Samanta(⁴), Poorvi Varshney(5)
(1) Associate Professor, Department of Medicine, Lady Hardinge Medical College, New Delhi
(2) Associate Professor, Department of Radiology, Lady Hardinge Medical College, New Delhi
(3) Senior Resident, Department of Medicine, Lady Hardinge Medical College, New Delhi
(⁴)Senior Resident, Department of Radiology, Lady Hardinge Medical College, New Delhi
(5) Junior Resident, Department of Medicine, Lady Hardinge Medical College, New Delhi
Abstract
We report a case who presented with long-standing fever, and investigations suggested abdominal tuberculosis. The patient was promptly initiated on anti-tuberculous therapy for 9 months. However, patient developed recurrence of symptoms after completing therapy. We discuss the scenarios in such a case.
Introduction
In clinical settings, at times it is difficult to obtain confirmatory evidence of a disease, and management needs to be started on clinical grounds and presumptive evidence. Situations can become dicey, when new symptoms arise, patients develop a complication or the treatment initiated fails. We discuss a similar clinical case scenario here.
Report of case
A 26-year male presented to Medicine OPD in June 2020 with complaints of fever with evening rise, loose stools, pain abdomen, and weight loss for 2months. Clinical examination did not reveal any potential diagnostic clues. CECT abdomen was consistent with features of abdominal tuberculosis (Figure 1) and the patient was started on anti-tuberculous therapy (ATT) in June 2020 after which he reported improvement in symptoms. Patient took regular ATT for 9 months.
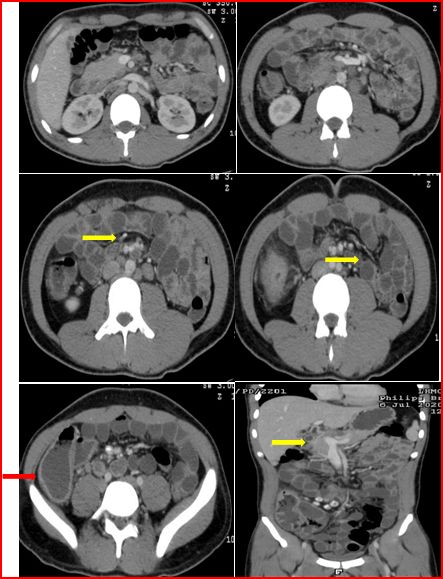
Figure 1- CECT abdomen shows circumferential focal ascending colonic wall thickening( red arrow) and enhancement with pericolic fat stranding. Terminal Ileum, ileo-caecal junction and caecal thickening with enteroliths. Abdominal lymphadenopathy (periportal, peripancreatic, mesenteric and retroperitoneal , yellow arrow)- necrotic as well as calcified are visible.
After 2-3 months of completing ATT, patient presented again in June 2021 with history of mass in right lower part of abdomen, pain abdomen and loose stools which started 1 month after discontinuation of ATT.Examination revealed a firm, mobile, non-tender mass of 5×5 cm in right iliac fossa. A repeat CECT abdomen was performed (Figure 2).CT scan was suggestive of tubercular etiology, asequela to abdominal tuberculosis (partial response).

Figure 2- CT abdomen revealing conglomerated lymph node mass in right iliac fossa (red arrow)with areas of necrosis and calcification. Persistence of thickening of terminal Ileum, ileocaecal junction and caecum (blue arrow).No evidence of ascending colonic wall thickening. Mild reduction in extent of mesenteric fat stranding in right iliac fossa. Persistence of abdominal lymphadenopathy (periportal, peripancreatic, mesenteric and RP)- increase in extent of calcification (decreased central necrosis). Right hydroureteronephrosis(black arrow)with upper ureteric calculus. No hepatic/splenic lesions seen. No stricture/fistula/abscess. Rest of the visualized bowel is shown to be normal (absence of multifocal involvement).
Discussion
This case is being discussed because such a case poses clinical dilemma and requires further investigation for its proper management. Tuberculosis is a common disease in tropical countries including India, and it is pertinent to understand its varied presentations specially extrapulmonary manifestations. Importantly, other diseases which can pose a differential to such a case should be known to the practitioners in general.
A possibility of partially treated tuberculosis or reactivation tuberculosis in this case is strong. Drug-resistant tuberculosis is also a possibility. However, it will be pertinent to think of alternative etiologies in the present scenario. Other causes of abdominal lymphadenopathy include infections (like HIV, Whippleʾs disease, enteric fever, EBV, etc.), inflammatory conditions (like inflammatory bowel disease, sarcoidosis, connective tissue disorders) and malignancies (lymphoma, abdominal malignancies, metastatic malignancies).
Causes of calcified abdominal lymph nodes include post-inflammatory tuberculosis being the most common, treated lymphomas, sarcomas and mucinous carcinomas. Lymph node necrosis is commonly seen in tuberculosis or suppurative conditions. Necrosis may also be seen in lymphomas and abdominal lymph node metastasis. Conglomeration of lymph nodes is seen in tuberculosis, and may also be seen in lymphomas and metastatic disease, and occasionally in fungal infections.
In this case the possibility of tuberculosis was given the highest priority. In initial CT, the presence of necrotic lymph nodes with calcification with bowel wall thickening and pericolic fat stranding were suggestive of infective/inflammatory condition. Following introduction of ATT there was a positive symptomatic response. Also, in repeat CT a reduction in necrosis and an increase in calcification of lymph nodes, absence of colonic wall thickening point towards a positive response to ATT. However, persistence of fat stranding and ileal, cecal, and ileocecal junction thickening points toward residual inflammation which can be due to partial response to ATT (requiring prolonging duration of ATT) or a drug resistant TB.
To confirm the diagnosis in such cases investigations ranging from routine blood analysis to tissue biopsy may be required. Complete blood count, serum biochemistry, ESR, Tuberculin skin test, Serum ACE levels, ANA, HIV, blood culture, chest-X ray, USG abdomen are often useful to support or refute a diagnosis. A very high ESR>100 is seen in tuberculosis, CTDs, lymphomas. Elevated ACE levels are seen in Sarcoidosis and disseminated tuberculosis. Bilateral hilar lymphadenopathy can be seen in tuberculosis, sarcoidosis, lymphoma and fungal infections. Sarcoidosis and tuberculosis have a predominant upper zone involvement and connective tissue disorders are predominant in lower zone. Due to these overlapping finding it often is difficult to distinguish them on preliminary investigations, and if the diagnosis is not clear we need to proceed with advanced radiological investigations and biopsy.
Tissue biopsy often yields a definitive diagnosis. External lymph nodes biopsy (if present) or image guided biopsy of internal lymph nodes can be done. Tissue sample must be analysed for Acid fast bacilli, CBNAAT, culture, histopathology and Drug susceptibility testing (if positive for tuberculosis).