An Interesting Case Of Collapsing Glomerulopathy Associated With Lichen Simplex Chronicus
Anurag Rohatgi(1), Farsana Mustafa(2), Saba Dabeer(3), Rahul Yadav(4), Kuldeep Kumar Gaur(5), Kaulali Sai Samarth(6), Rahul Sangwan(7)
(1) Director Professor, Department of Medicine, Lady Hardinge Medical College, New Delhi
(3) Senior Resident, Department of Medicine, Lady Hardinge Medical College, New Delhi
(2,5) Post Graduate Student, Department of Medicine, Lady Hardinge Medical College, New Delhi
(4,6,7) Post Graduate Student, Department of Medicine, Atal Bihari Vajpayee Institute of Medical Sciences, New Delhi
ABSTRACT
Collapsing Glomerulopathy is a devastating Clinical and Pathological variant of Focal Segmental Glomerulosclerosis which can relentlessly progress to End stage Renal disease. Lichen Simplex Chronicus is primarily a Neurodermatitis characterized by an itch scratch cycle. We report a Case of Collapsing Glomerulopathy closely associated with the onset of Lichen Simplex Chronicus in a 27 year old Male. This case invoked a thought process in our minds whether both these conditions are coincidental or related to each other. Despite a wide literature search no Articles were found establishing the presence of Lichen Simplex Chronicus along with Collapsing Glomerulopathy.
Keywords -Collapsing Glomerulopathy, Lichen Simplex Chronicus
INTRODUCTION
Collapsing Glomerulopathy is a Pathologically and Clinically distinct variant of Focal Segmental Glomerulosclerosis characterized by a rapid clinical course with a high incidence of Nephrotic syndrome, Rapidly progressive Renal failure and relative resistance to standard treatment1. Lichen Simplex Chronicus is characterized by Thickening and Hyperpigmentation of the Skin with variable Scaling. It is secondary to repetitive scratching of Skin. Both these disorders have wide range of triggering factors.
Most cases of Collapsing Glomerulopathy not associated with HIV infection are considered to be idiopathic. In one series of 88 patients published by Nicholas Cossey, 77 percent were found to be Idiopathic2. This large burden of so called ‘Idiopathic’ cases may be associated with uncharacterized Infectious triggers. Here we had an interesting case of Collapsing Glomerulopathy which manifested in close temporal relationship with the onset of Lichen Simplex Chronicus.
CASE REPORT
A 27 year old Nonobese Male presented with complaints of Pedal Edema and Facial Puffiness of 25 days duration. He also complained of frothiuria for 20 days and breathlessness with anorexia for 2 weeks. 1 month before these complaints, he noticed a Skin lesion on right Shin and he also experienced persistent Itching over it. No history of Hematuria, decreased Urine output, Abdominal distension, Fever or Pharyngitis was reported with or before the illness. He denied history of prior Medication, Blood transfusion or Intravenous drug use. The relevant Clinical Examination findings and preliminary Investigations of our patient are given in Table 1 & Table 2.
TABLE 1

TABLE 2
| Hemoglobin;TLC;PLT Count;ESR | 11.6 gm%;7800cumm;1.7Lakh;35 mm |
| Peripheral smear | Normocytic Normochromic RBCs, platelet count adequate |
| Blood urea;Serum Creatinine | 103mg/dl;5.8 mg/dl |
| Serum protein/albumin | 5.2 gm/dl / 2.6gm/dl |
| Calcium/ phosphorous | 9 mg/dl/ 3.5 gm/dl |
| Fasting Triglycerides;Cholesterol;HDL;LDL | 141 mg/dl;273 mg/dl;67mg/dl;177mg/dl |
| Arterial blood gas analysis | Normal |
| Urine Routine Microscopy | 2-5 pus cells/ high power field, 20-25 RBCs, protein 2+, occasional granular casts |
| 24 hour Urine protein | 3210 gm/day |
| C3;C4
|
122 mg/dl (66 to 185 mg/dl); 24 mg/dl (15 to 52 mg/dl) |
| Antinuclear antibody
Extended ANA profile |
Negative
Negative |
| c ANCA, p ANCA, Anti GBM | Negative |
| RA factor, ASO titres | Negative |
| Hepatitis B surface antigen, VDRL, Anti HCV antibody | Negative |
| COVID 19 RT PCR | Negative |
| HIV (ELISA) | Negative |
| Blood culture, Urine culture, Throat culture | Sterile |
| Ultrasound Whole abdomen | Right kidney size 10.6*3.9 cm and Left kidney size 10.8*4 cm, Raised Cortical Echogenecity and partially lost Corticomedullary differentiation. |
| Renal Doppler | No evidence of Thrombosis in renal vessels |
After reviewing the reports we planned to proceed with a Renal biopsy. Meanwhile, a Dermatology opinion, taken for the Skin lesion shown in figure 1 suggested a differential diagnosis of Lichen Amyloidosis or Lichen Simplex Chronicus and a Skin biopsy was advised from the Skin lesion.
SKIN BIOPSY
Epidermis showed hyperkeratosis, prominent Granular layer, moderate Acanthosis with prominent Basal layer pigmentation. Papillary dermis revealed fibrosis with vertical streaking of collagen bundles and moderate perivascular mononuclear infiltrate. No Amyloid deposits were seen. Biopsy findings in the Dermatologist’s opinion were conforming to Lichen Simplex Chronicus.

Figure1. Skin lesion on Right shin
KIDNEY BIOPSY
A light microscopic examination of Renal biopsy showed nine Glomeruli which was showing expansion of the Bownman space, proliferation of Parietal Podocytes and Glomerular tuft collapse. There was increase in Mesangial matrix and Cellularity. Silver Methanamine staining showed focal splitting of Glomerular basement membrane. There was significant Tubulointerstitial injury as evidenced by Microcystic Tubular dilatation; prominent reabsorption granules in the Tubules; lowering of Epithelium and focal Acute tubular necrosis. Interstitium showed Edema and diffuse Chronic inflammatory infiltrates. Medium sized vessels showed prominent Medial Sclerosis and duplication of Internal Elastic Lamina. 50 % of Tubulointerstitial component showed Chronic parencymal damage on MT stain (Figure 2). Immunofluroscence showed weak nonspecific Glomerular IgM deposits with no C3, C1q, IgG, IgA or Fibrin deposits. Electron microscopy showed marked wrinkling of Glomerular basement membrane with occlusion of Capillary lumens, Visceral epithelial hypertrophy, Foot process fusion and detachment of Podocytes from GBM.

Figure 2. Histopathology slides. (A) Light microscopy 40X image showing enlarged Glomeruli with proliferation of Parietal podocytes, Glomerular tuft collapse. (B) Light microscopy 10X image showing increase in Mesangial Matrix and cellularity.

Figure 2. (C) Periodic acid-Schiff stain 40X :Tubules showing prominent resorption granules. Dilatation of Tubules to form Microcystic change. (D) Interstitium showing edema and diffuse chronic inflammatory cell infiltrate and focally admixed with Eosinophils and Polymorphs.
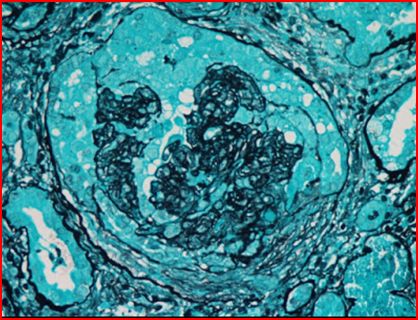
Figure 2. (E) Silver Methanamine stain: showing focal splitting of Basement membrane

Figure 2. Masson’s trichrome (F) 10X and (G) 4X view: 50 percent of Tubulointerstitial compartment showing Chronic Parenchymal damage.
CLINICAL COURSE
In Consult with Nephrologist, the patient was given 3 doses of Methylprednisolone followed by oral Prednisolone (40mg OD) and MMF 500mg 1.5Tab twice daily. An extensive Etiological workup was done for the all feasible Infectious agents including COVID 19. Parvovirus B19 Serology and Genetic studies couldn’t be done due to Logistic and Financial constraints.
He was discharged on this as he was not having any Uremic symptoms and asked to follow up in OPD. However, he did not report for follow up. He was admitted 1 month later again in a state of altered Sensorium. Attendants informed that he had got 1 session of Hemodialysis from another Hospital. 2 days following that session, he developed sudden onset altered Sensorium. At the Emergency ward, NCCT Head was ordered which revealed Posterior Reversible Encephalopathy syndrome and Hyperdensity of Blood attenuation along leaflet of Left Tentorium Cerebelli, suggestive of likely SDH. His KFT reports were in the range of ESRD. He succumbed soon after.

Figure 3. Ill defined White Matter hypodenties seen in Bilateral Occipital Lobes suggestive of Posterior Reversible Encephalopathy Syndrome. Hyperdensity of Blood Attenuation seen along leaflet of Left Tentorium Cerebelli: likely Subdural Hematoma.
DISCUSSION
Collapsing Glomerulopathy is an aggressive form of FSGS characterized by Black Racial predominance, relatively Rapid progression of Renal insufficiency, Massive Proteinuria, distinct Histopathological features and poor response to Immunosuppressive agents. Apart from HIV there are multiple Etiological factors associated with this Pathological entity3(Table 3). However no one definable Pathogenic trigger for Collapsing Glomerulopathy has emerged clearly4.

Collapsing Glomerulopathy has been shown to be associated with Homozygous APOL1 risk Alleles. Glomerular injury and inflammatory second hits can precipitate kidney damage in patients with APOL1 risk factors2. As genetic screening is not feasible in Low Socioeconomic settings, possible Inflammatory and Infectious conditions which can trigger this “Second hit” in APOL1 risk variants should alert the Clinician for periodic monitoring of kidney functions in such Individuals. Morphological features in the kidney biopsy which can point towards underlying APOL1 Gene risk variants include a combination of Microcystic Tubular dilatation, Thyroid type Tubular atrophy and a predominance of Solidified /disappearing type Global Glomerulosclerosis5. This specific constellation of Histopatholopathological findings can be utilized in our settings where we can retrospectively decide regarding the screening for mutations in such patients. In our case we excluded all possible Infectious triggers of Collapsing Glomerulopathy (except Parvovirus B19 because of Logistic constraints and moreover patient’s clinical profile was not suggestive of this infection).
In our case 1 month before the onset of symptoms, he had Skin lesions on right Shin associated with pruritis. The Skin lesion Clinically and Histopathologically suggested the diagnosis of Lichen Simplex Chronicus. Patients suffering from generalized pruritis in the absence of Primary Skin disease will usually be evaluated for Systemic diseases. But in contrast to this, localized pruritis resulting in Lichen Simplex Chronicus is rarely investigated6. The most frequent General disorders related to this in Literature are described in table 47. Our patient progressed to End stage Renal disease within a 1 month span and developed uremic bleed and succumbed to death.
Table4: Systemic diseases with a higher prevalence of Lichen Simplex Chronicus

In our case we had a temporal relationship between onset of Lichen Simplex Chronicus and Collapsing Glomerulopathy. Though increased prevalence of Chronic Kidney disease has been described in Lichen Simplex Chronicus patients, even an extensive literature search couldn’t bring out any association of Lichen Simplex Chronicus and Collapsing Glomerulopathy. In this context, whether it was a coincidental occurrence of two separate diseases or both these conditions had a common unknown Infectious trigger requires further research. More such Case reports and research will be required for enhancing our knowledge regarding this aspect.
References
- Albaqumi M, Soos TJ, Barisoni L, Nelson PJ. Collapsing glomerulopathy. Journal of the American Society of Nephrology. 2006 Oct 1;17(10):2854-63.
- Nicholas Cossey L, Larsen CP, Liapis H. Collapsing glomerulopathy: a 30-year perspective and single, large center experience. Clinical kidney journal. 2017 Aug 1;10(4):443-9.
- Chandra P, Kopp JB. Viruses and collapsing glomerulopathy: a brief critical review. Clinical kidney journal. 2013 Feb 1;6(1):1-5.
- Albaqumi M, Barisoni L. Current views on collapsing glomerulopathy. Journal of the American Society of Nephrology. 2008 Jul 1;19(7):1276-81.
- Larsen CP, Beggs ML, Saeed M, Ambruzs JM, Cossey LN, Messias NC, Walker PD, Freedman
- Histopathologic findings associated with APOL1 risk variants in chronic kidney disease. Modern pathology. 2015 Jan;28(1):95-102.
- Gach JE, Seddon HF. Gluten-sensitive enteropathy associated with genital lichen simplex chronicus. JRSM short reports. 2010 Oct;1(5):1-3.
- 8.Juan CK, Chen HJ, Shen JL, Kao CH. Lichen simplex chronicus associated with erectile dysfunction: a population-based retrospective cohort study. PLoS One. 2015 Jun 15;10(6):e0128