Saba Dabeer (1), Anurag Rohatgi (2)
(1)Post Graduate Resident, Department of Medicine, Lady Hardinge Medical College and Associated Hospitals, New Delhi
(2)Director Professor, Department of Medicine, Lady Hardinge Medical College and Associated Hospitals, New Delhi
ABSTRACT
Background: Worldwide, headache disorders have been labelled as one of the leading causes of morbidity.It is, paradoxically, a burden widely ignored.
Objectives: To determine clinical profile and headache type distribution of chronic primary headache disorders.
Methods: A cross-sectional observational study was conducted in the Department of Medicine, LHMC and Associated hospitals, New Delhi.70 patients were administered a structured questionnaire and their responses were recorded.
Results: Among the 70 patients, females (61.4%) outnumbered males (38.5%). Prevalence (44%) was highest in productive age groups (21 to 30 years). Tension-type headache (4.43%) was the most common type followed by Migraine (24.29%). Majority of the patients were housewives (58.5%). Stress was found to be the most common precipitating factor (18.5%) while sleep (51%) served as the most common relieving factor.
Conclusions and Recommendations: A great lacuna exists for the holistic approach in patient management in centers like ours where not much time is given to the counseling and education of patients. We henceforth, suggest that separate headache clinics should be set up to address these issues.
BACKGROUND
“Every head has its own headache.”
Headache has been one of the most common maladies to affect mankind. 76% of women and 57% of men report at least one significant headache per month, and more than 90% experience at least one noteworthy headache in their lifetime. (1)
It is, paradoxically, a burden widely ignored. The following conclusion appeared in the Atlas of Headache Disorders and Resources in the World 2011(2), published by the World Health Organization (WHO): “The facts and figures [on headache] illuminate worldwide neglect of major causes of public ill-health, and the inadequacies of responses to them in countries throughout the world.”
An article by Dr. K. Ravishankar and Dr. A. Chakravarty, “Headache-The Indian Experience” (2002) says: “I would like to make some pleas to my colleagues. Headache in India is as important as any other neurological problem, and yet it is neglected by the medical community. The study of headache is relatively simple and cheap compared to other neurological disorders. Prevalence data are essential. To prevent misconceptions among doctors and to promote research, headache must be given greater importance in the medical curriculum.”(22)
The International Classification of Headache Disorders (ICHD) was first published in 1988 and has now gone through two revisions, most recently in 2013. Headache disorders have been classified into PRIMARY AND SECONDARY by the International Headache Society (3). Primary headaches are those in which headache and its associated features are the disorder, whereas secondary headaches are those caused by exogenous disorders (4). The International Classification of Headache Disorders (beta version), 3rd edition (2013) has further classified primary headache disorders into – Migraine, Tension-type headache, Trigeminal autonomic cephalagias and other primary headache disorders. (3)
The type of most headaches can be determined by a careful history and physical examination. The clinical imperative is to recognize the warning signals that raise red flags and prompt further diagnostic testing. If the patient does not respond to conventional therapy, the diagnosis of primary headache should be questioned and the possibility of secondary headache disorder should be revisited.(5)
Knowing the headache profile of patients attended to, in tertiary centers may help the preparation of diagnostic and therapeutic processes at the primary and secondary care levels, enabling a more suitable treatment of the cases.(6) Henceforth, in the current study, we tend to determine the clinical profile and etiological distribution of chronic primary headache disorders that is, headache for a period of at least 3 months,(7) among patients attending a tertiary care center.
METHODS
An institution based cross-sectional observational study was conducted from November 2017 to April 2019in the Department of Medicine, LHMC and Associated Hospitals, New Delhi. Due clearance was obtained from the ethical committee beforehand.
A total of 70 patients fitting into the criteria of Chronic Primary Headache Disorders were included in the study after taking written informed consent. A structured proforma was used that included self-administered questions. Results were recorded.
Data were entered into a secured database and statistical analysis was performed using SPSS software.
RESULTS
Mean age of the study population was 31.11 years with a standard deviation of 6.92 years. Age Range of the population was 18-44 years. Median was 30 years.
43 (61.43%) of them were females and 27 (38.57%) were males.
Out of 70 patients, 29 (41.43%) patients had “tension type” of headache, 14 patients (20%) had “Migraine with aura” while 10 (14.20%) patients suffered from “Migraine without aura”. Remaining 17 (24.29%) were classified into “others” category.
Out of the 70 patients, 50 were married, 14 were unmarried while others were divorced/ had separated/ or widowed.
In the population studied, 40% could not identify a trigger factor, 12.86% had exercise as the trigger factor, 28.57% had other triggers such as computer work; fatigue; little sleep and 18.57% identified stress as a trigger factor.
In the study population 36;14;11 people reported that sleep; rest; medications were the relieving factors respectively, while 9 told that staying in a quiet, dark room relieved their headache.
Out of 70 patients, 26 patients had been suffering with headache for past 1 year, 20 patients for more than 1 year but less than 2 years, 16 patients for more than 2 years but less than 3 years and 8 patients for more than 3 years.
The study population was distributed into medication usage based on the number of pills used per month for relief. Majority (28.57%)of patients took 11-15 pills per month while 15.71% took no pills.
65 patients had no similar family history while 5 of the patients had family history of similar complaints.
50 patients (71.43%) had no stress while 19 patients (27.14%) did have stress and one patient recorded no entry.
Out of70 patients, 24 were suffering from migraine out of which 14 (58.33%) had symptoms of aura while 10 patients (41.67%) had no such symptoms. Out of 14 patients diagnosed with “Migraine with Aura”, 10 had visual warning symptoms while 4 had auditory symptoms.
Out of 70 patients, 14 patients (20%) were housewives while there were 10 students (14.29%).
Majority (17 patients;24.29%) reported a family income of more than 2 lakhs but less than 4 lakhs.
Majority(48 out of 70)patients had normal BMI, 8 were overweight, 9 patients were pre-obese while 5 of them were obese.
Out of 24 patients of migraine, 9 were in the range of 25-30 years, followed by 5 in the range of 30-35 years. Out of 29 patients with tension-type headache, 8 patients were in the range of 25-30 years while 6 were in the range of 30-35 years. It was also found that majority (17 out of 24) migraineurs were females, while majority (16 out of 29) diagnosed with tension-type as headache type were males.
DISCUSSION
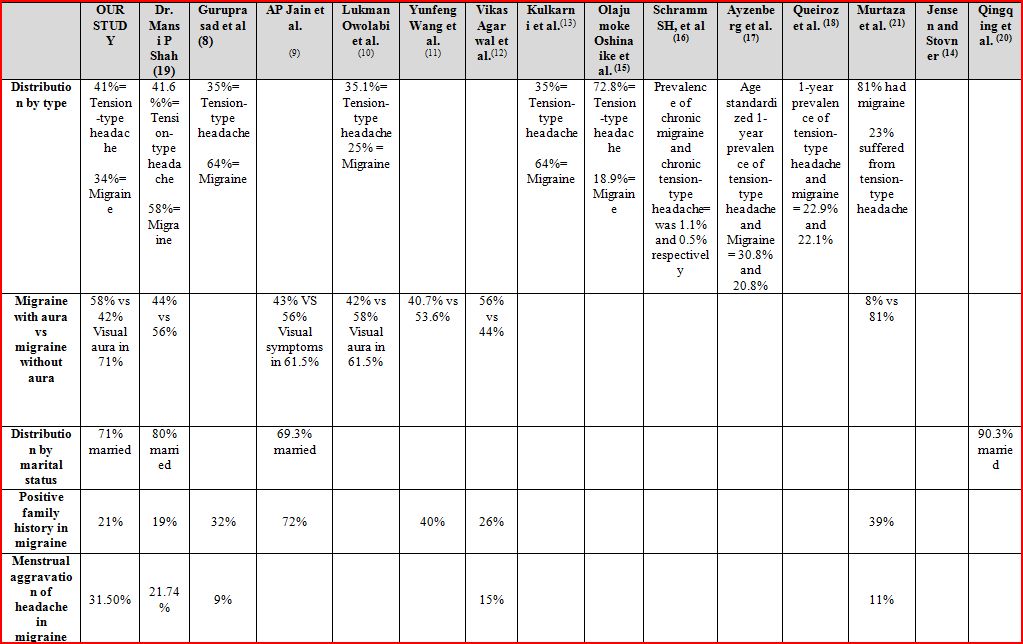
The results obtained were compared with other studies conducted in different places and at different times. In the present study, amongst the 70 patients, the peak prevalence of chronic primary headache was seen in 21 to 30 years age group, similar to those made by studies carried out at different places and at different times. Amongst the 70 patients, females outnumbered males. 38.6% of patients were males while 61.4% of them were females. Amongst the patients suffering from migraine, 29% were males while 71% were females (male: female ratio being 1:2.4). These observations were similar to some studies carried out in India and elsewhere. On the other hand, out of 29 patients suffering from tension-type headache, 45% were females while 55% were males (male: female ratio being 1.2:1); contrary to what was observed in studies elsewhere. In our study, amongst the 70 patients enrolled, 34% of the patients had migraine while 41% of them were suffering from tension-type headache, again similar to other studies except the one by Murtaza et al. (21)
Tension-type headache has been observed in higher prevalence than migraine in most of the population-based studies. However, in hospital-based studies reported from India, prevalence of migraine and tension-type headache has been variable. In case of migraine, it ranges from 13.6% to 78% (96). 71% of patients enrolled were married while 20% were unmarried, which is in conformity with reports from studies conducted in different places and at different times. In the current study, 48.5% patients were housewives while 11% were students in order of prevalence. 54% migraineurs were housewives while 34% patients with tension-type headache were housewives, similar to what other studies in India have reported. In the present study 18.57% of patients with chronic primary headache disorders had stress as precipitating factor. In a study by Dr. Mansi P Shah (19), stress precipitated symptoms in 45% of patients presenting with headache. 26.4% of patients with migraine plus tension type headache had symptoms aggravated due to stress according to a study by Vikas Agarwal et al. (12)In the current study sleep (51%) was the most common relieving factor followed by rest (20%), medications (15.7%) and dark quiet room (13%).
In a study by Olajumoke Oshinaike et al. (15), the common relieving factors were rest in 57.4% and analgesic use in 31%. A study by Dr. Mansi P Shah (19), reported that use of analgesic medications served as relief from headache in 34% patients followed by dark quiet surroundings in 14%.



CONCLUSIONS AND RECOMMENDATIONS
There is a dearth of studies in India regarding clinical profile of chronic primary headache disorders. Our study can act as a stepping zone for further larger studies in India. Many of our results were resonant with those of studies done at different times and in different places, both in India as well as outside India. This study, thus, adds to the already existing literature.
However, being a hospital-based study, its results cannot be extrapolated to study the prevalence of primary headaches in the general population. Also, since we compared only a limited number of clinical features in tension-type headache and migraine, further studies will be needed to differentiate these two.
We, our study being the first step of a long journey, would like to make certain recommendations. Migraine and tension-type headache are separate entities that need to be dealt differently. Our study included only 70 patients and was a single-center study. Henceforth, a multicentric study comprising a large number of patients should be done to gain more information about the clinical profile of chronic primary headache patients. A great lacuna exists for the holistic approach in patient management in centers like ours where not much time is given to the counseling and education of the patients and their attendants. We, henceforth, suggest that separate headache clinics should be set up to address these issues.
REFERENCES
- Saper JR. Headache disorders. Medical Clinics of North America. 1999 May 1;83(3):663-90.
- World Health Organization. Atlas of headache disorders and resources in the world 2011
- Headache Classification Committee of the International Headache Society (HIS. The International Classification of headache disorders, (beta version). Cephalalgia.2013 Jun 14
- Kasper DL, Fauci AS, Hauser S, et al, editors. Harrison’s principles of internal medicine, 19th ed.
- Silberstein SD. Chronic daily headache: diagnosis and treatment. Headache in clinical practice. 1998
- Chakravarthy A. Pitfalls in the diagnosis of primary headaches; Annuals of Indian academy of Neurology. 2002;5: 13-9.
- Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton RB, Scher AI, Steiner TJ, Zwart JA. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007 Mar;27(3):193-210.
- Guruprasad KG, Dadapeer K, Niranjan MR. Sociodemographic profile, classification and clinical profile of headache–a semiurban hospital-based study. J Clin Diag Res. 2012; 6:278-81
- Jain AP, Chauhan B, Bhat AD. Sociodemographic and clinical profile of headache–a rural hospital-based study. Hypertension. 2007;1:0-49.
- Nigeria N. Clinical Profile of Primary Headache disorders in Kano, Northwestern Nigeria. Journal of Medicine in the Tropics. 2012;14(2):109-15.
- Wang Y, Zhou J, Fan X, Li X, Ran L, Tan G, Chen L, Wang K, Liu B. Classification and clinical features of headache patients: an outpatient clinic study from China. The journal of headache and pain. 2011 Oct;12(5):561.
- Agarwal VI, Chaurasia RN, Mishra VN, Joshi DE, Misra SU. Clinical profile of headache from a tertiary care centre in eastern India. International journal of general medicine and pharmacy (IJGMP). 2013;2(3):9-14.
- Rao GN, Kulkarni GB, Gururaj G, Stovner LJ, Steiner TJ. The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State. The journal of headache and pain. 2015 Dec;16(1):94.
- Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. The Lancet Neurology. 2008 Apr 1;7(4):354-61.
- Oshinaike O, Ojo O, Okubadejo N, Ojelabi O, Dada A. Primary headache disorders at a tertiary health facility in Lagos, Nigeria: prevalence and consultation patterns. BioMed research international. 2014;2014.
- Schramm SH, Obermann M, Katsarava Z, Diener HC, Moebus S, Yoon MS. Epidemiological profiles of patients with chronic migraine and chronic tension-type headache. The journal of headache and pain. 2013 Dec;14(1):40.
- Ayzenberg I, Katsarava Z, Mathalikov R, Chernysh M, Osipova V, Tabeeva G, Steiner TJ, Lifting The Burden: the Global Campaign to Reduce Burden of Headache Worldwide and the Russian Linguistic Subcommittee of the International Headache Society. The burden of headache in Russia: validation of the diagnostic questionnaire in a population‐based sample. European journal of neurology. 2011 Mar;18(3):454-9.
- Queiroz LP, Peres MF, Piovesan EJ, Kowacs F, Ciciarelli MC, Souza JA, Zukerman E. A nationwide population-based study of migraine in Brazil. Cephalalgia. 2009 Jun;29(6):642-9.
- Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population—a prevalence study. Journal of clinical epidemiology. 1991 Jan 1;44(11):1147-57.
- Huang Q, Yu H, Zhang N, Guo B, Feng C, Wang S, Liang X. Body Mass Index and Primary Headache: A Hospital-Based Study in China. BioMed Research International. 2019;2019.
- Murtaza M, Kisat M, Daniel H, Sonawalla AB. Classification and clinical features of headache disorders in Pakistan: a retrospective review of clinical data. PloS one. 2009 Jun 8;4(6):e5827.
- Ravishankar K, Chakravarthy A. Headache – the Indian experience. Annals Indian Acad Neurol. 2002;5:107–112