https://meditropics.com/1568-2/
*Usha Srinag
*Post Graduate Resident, Department of Medicine, LHMC
Abstract:
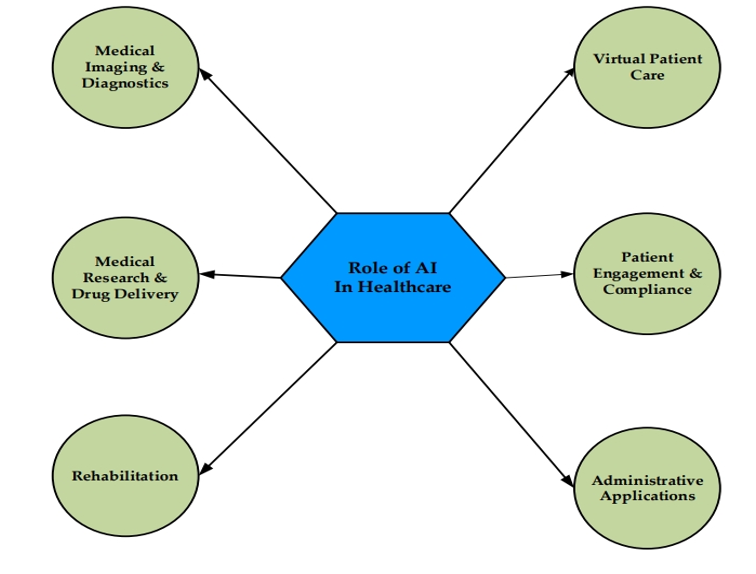
This review explores the evolving role of artificial intelligence (AI) in healthcare, highlighting its potential to enhance diagnostic accuracy, streamline clinical workflows, and improve patient outcomes. Key applications of AI, including machine learning (ML) and deep learning (DL), are discussed across various medical fields such as cardiology, neurology, and endocrinology. The article addresses challenges like data limitations, algorithmic bias, and the need for robust regulatory frameworks. While AI promises transformative advancements, its integration must prioritize ethical considerations and complement human expertise. The future of AI in healthcare lies in a balanced, synergistic approach between technology and clinical practice.
Introduction:
The journey of artificial intelligence (AI) began with Alan Turing’s groundbreaking ideas in 1950, where he introduced the Turing test to assess a machine’s ability to exhibit intelligent behaviour akin to that of humans. Just six years later, John McCarthy coined the term “artificial intelligence,” framing it as the science and engineering of creating intelligent machines. Over the decades, AI has evolved from simple “if, then” rules to intricate algorithms that mirror the complexities of the human brain. Among its many subfields, machine learning (ML) stands out as a powerful tool that identifies patterns and enables machines to learn from data, allowing for dynamic clinical decision-making that tailors patient care to individual needs rather than relying on static protocols (1). The integration of AI into healthcare has opened up unprecedented opportunities for improving patient outcomes, streamlining clinical workflows, and accelerating medical research. Recent years have witnessed remarkable progress in AI applications across various medical specialties. From disease risk assessment and treatment prediction to complication management and patient care support, AI is reshaping the way healthcare is delivered and experienced.
Artificial Intelligence in Medicine:
In modern discourse, “AI” is frequently used to describe Machine Learning (ML), where algorithms are applied to analyse data, learn from feedback, and enhance their accuracy. For instance, algorithms can be crafted to detect anomalies in x-ray images or patient symptoms, improving their precision based on clinician feedback regarding true or false positives and negatives. Deep Learning (DL) advances this concept by structuring algorithms in layers, forming artificial neural networks that can autonomously learn and make intelligent decisions. The “FUTURE of Artificial Intelligence Act of 2017” in the U.S. defines “general AI” as systems exhibiting human-like intelligence across cognitive, emotional, and social behaviours, while “narrow AI” pertains to specific applications like language translation and autonomous vehicles (2).
In the realm of medicine, AI can be divided into virtual and physical categories. Virtual AI includes systems like electronic health records and neural networks that assist in making treatment decisions, enhancing the decision-making process with data-driven insights. Physical AI, on the other hand, encompasses technologies such as surgical robots, intelligent prosthetics, and devices for elderly care, which directly interact with patients to improve healthcare delivery. In this context, computers employ two primary diagnostic techniques: the flowchart approach and the database approach. The flowchart approach simulates a physician’s diagnostic process by asking a series of questions to arrive at a probable diagnosis, but it is limited by the machine’s inability to perceive subtle cues during patient interactions that a doctor would naturally observe. Conversely, the database approach utilizes deep learning and pattern recognition, where computers are trained through repetitive algorithms to identify specific symptom patterns or clinical images (3).
Current Applications of Artificial Intelligence in Medicine:
AI in medicine has seen significant advancements with several FDA approvals for various applications. In cardiology, AliveCor received FDA approval in 2014 for its Kardia mobile app, enabling smartphone-based ECG monitoring for early detection of atrial fibrillation (AF). Similarly, Apple obtained FDA approval for its Apple Watch 4, which allows users to acquire ECG readings and detect AF, sharing results with healthcare providers. In endocrinology, Medtronic’s Guardian system, approved by the FDA, offers continuous glucose monitoring for diabetes patients, syncing with smartphones. In 2018, Empatica gained FDA approval for its Embrace wearable device, which detects generalized seizures in epilepsy patients and alerts their caregivers via a mobile app. Additionally, Paige.ai received breakthrough status from the FDA for its AI-based algorithm capable of diagnosing cancer in histopathology with high accuracy, helping pathologists prioritize critical slides. These approvals mark important milestones in integrating AI into clinical practice across multiple specialties (4). IBM Watson Health’s real-time monitoring system was designed using IBM Cloud and AI technology. It integrates and analyzes large amounts of data from a variety of devices to help healthcare institutions and mental health professionals monitor and analyze patients’ mental states in real time (5).
The doctor’s hand remains the most essential tool for examining a patient, as no AI can replicate the human touch. Following this, the stethoscope is the next critical piece of clinical equipment, which has been enhanced by AI technology. Digital stethoscopes now integrate AI to improve diagnostic accuracy and aid in cases where auscultation skills may be lacking. AI-based models have been developed to analysed auscultation data for identifying valvular stenotic lesions. Additionally, lighter and more affordable models have been created to detect cardiac and pulmonary sounds. A recent deep learning system, AI-ECG, analysed single-lead ECGs collected during clinical exams using an ECG-enabled stethoscope. Numerous other AI applications in clinical evaluation have emerged recently. For example, a study identified Parkinson’s disease using voice signals, achieving high accuracies of 98.3% and 95% with multilayer perceptron (MLP) and support vector machine (SVM) models, respectively.
AI has the potential to significantly enhance the differential diagnosis process by meticulously analysing patient data and generating a list of possible diagnoses along with the likelihood of each. Utilizing artificial neural networks (ANNs), patient data can be stratified into various risk categories for different diseases. For instance, one ANN model has been developed to predict pancreatic cancer with an 80.7% sensitivity and specificity, effectively categorizing patients into low, medium, and high-risk groups. Tools like Isabel DDx Companion and Glass AI exemplify AI’s role in differential diagnosis, with large language models such as GPT-4 also assisting clinicians in this critical task. AI has also played a crucial role in ischemic stroke management, enabling early stroke diagnosis, automated calculations of the Alberta Stroke Program Early CT Score (ASPECTS), and evaluation of ischemic core and penumbra. Its utility extends to detecting and classifying neurological disorders, including Alzheimer’s disease and brain tumors, using MRI data, often surpassing radiology residents and fellows in accuracy (6).
Artificial Medicine in Medical Education:
AI offers various transformative methods for medical education, enhancing both personalized and experiential learning. By tailoring learning experiences based on individual strengths and weaknesses, AI-driven adaptive platforms create customized paths for students. Virtual patient simulations and AI-powered intelligent tutoring systems allow learners to engage with realistic clinical scenarios and receive immediate feedback, aiding in clinical decision-making. Automated assessment tools provide instant, detailed feedback, while natural language processing facilitates quick access to medical literature and case studies (7). Additionally, AI enhances virtual and augmented reality experiences, simulating surgeries and patient interactions for immersive learning. Predictive analytics can help educators refine curricula by analyzing data on student outcomes, while AI chatbots provide 24/7 support, answering questions and guiding learners through resources. Data-driven insights reveal successful teaching methods and highlight areas for improvement. Furthermore, AI-generated interdisciplinary case studies integrate fields like radiology and pharmacology, offering holistic learning experiences that prepare students for the complexities of real-world healthcare. These AI-driven approaches not only improve educational effectiveness but also familiarize students with the AI tools they will use in clinical practice (8).
Challenges in AI in Medicine:
The use of AI in healthcare presents numerous challenges that hinder its full potential. Many AI models, while promising, are trained on retrospective data, leading to a drop in performance when faced with real-world, unseen data. Moreover, the lack of validation through randomized controlled trials (RCTs), the gold standard in medicine, further complicates their clinical adoption. Common performance metrics such as accuracy and AUC often fail to capture the true impact of AI in clinical settings, and the inconsistency in methods, datasets, and metrics across studies makes comparing different algorithms difficult (9). Additionally, AI models are vulnerable to dataset shifts, where changes in data over time or between locations reduce their reliability, necessitating constant updates and recalibrations. There are also concerns about AI picking up irrelevant signals or confounding factors, which can lead to incorrect conclusions. The ability to generalize across diverse populations remains a significant obstacle, with many models underperforming in different geographic or demographic settings. Algorithmic bias, where AI systems reinforce existing disparities, is a critical issue, particularly in minority subgroups. Furthermore, AI systems can be susceptible to adversarial attacks, where small manipulations of input data can lead to erroneous decisions. The fragmented nature of healthcare data, often siloed across systems, presents logistical challenges, while regulatory frameworks struggle to keep pace with rapid innovations in AI. Finally, human barriers, such as clinicians’ hesitancy to trust or integrate AI into their workflow, underscore the importance of transparency, interpretability, and alignment with clinical needs (10).
Conclusion:
In conclusion, the integration of artificial intelligence into healthcare holds immense promise, yet its path to full adoption is paved with both opportunity and caution. While AI has the potential to revolutionize medical practice by enhancing precision, reducing errors, and empowering patients in their own care, its success depends on the thoughtful balance of innovation with ethical and practical considerations. Rigorous validation, robust regulatory frameworks, and the continuous involvement of human expertise remain paramount to ensure that AI complements, rather than replaces, the nuanced judgment of clinicians. As AI systems evolve, their capacity to transform healthcare will likely be realized not in sweeping changes, but through gradual, well-monitored advancements that enhance both clinical outcomes and patient experiences. Ultimately, the future of AI in healthcare rests on its ability to harmonize cutting-edge technology with the irreplaceable human touch, crafting a synergistic model that serves both patients and providers.
REFERENCES:
- Kaul V, Enslin S, Gross SA. History of artificial intelligence in medicine. Endosc. 2020;92(4):807-12.
- Greenhill AT, Edmunds BR. A primer of artificial intelligence in medicine. 2020 ;22(2):85-9.
- Malik P, Pathania M, Rathaur VK. Overview of artificial intelligence in medicine. J. Fam. Med. Prim. Care. 2019;8(7):2328-31.
- Briganti G, Le Moine O. Artificial intelligence in medicine: today and tomorrow. Front. Med. 2023; 7:509744.
- Suo N. Watson for the Cloud: How IBM is Leading the Way in Medical AI Research and Development AI-Powered Mental Health Monitoring: Artificial Intelligence for Medicine Science 2023. 1: 811-817.
- Krishnan G, Singh S, Pathania M, Gosavi S, Abhishek S, Parchani A, et al. Artificial intelligence in clinical medicine: catalyzing a sustainable global healthcare paradigm. Front. Artif. Intell. 2023; 6:1227091.
- Karalis VD. The integration of artificial intelligence into clinical practice. Appl. Biosci. 2024;3(1):14-44.
- Han ER, Yeo S, Kim MJ, Lee YH, Park KH, Roh H. Medical education trends for future physicians in the era of advanced technology and artificial intelligence: an integrative review. BMC. Med. Edu. 2019; 19:1-5.
- Jiang L, Wu Z, Xu X, Zhan Y, Jin X, Wang L, et al. Opportunities and challenges of artificial intelligence in the medical field: current application, emerging problems, and problem-solving strategies. J. Int. Med. Res. 2021;49(3):03000605211000157.
- Kelly CJ, Karthikesalingam A, Suleyman M, Corrado G, King D. Key challenges for delivering clinical impact with artificial intelligence. BMC.Med. 2019;17:1-9.